Abstract
Abstract 932
With increasing scrutiny of healthcare expenditures, the reduction of hospital readmission rates has emerged as a targeted area of health reform; however, readmission rates following hematopoietic cell transplantation (HCT) have not been systematically examined. Whereas patients (pts) undergoing allogeneic HCT at increased risk of toxicity and mortality can be identified by their coexistent medical comorbidities as calculated by the HCT-comorbidity index (HCT-CI), the impact of such pre-HCT characteristics on outcome following high dose chemotherapy with autologous HCT is not known. We retrospectively analyzed the association of pre-transplantation HCT-CI with readmission rates and survival for all pts who underwent autologous HCT at a single institution from 1/2004 to 12/2008.
Of 475 pts who underwent an autologous HCT, 62% were male and the median age was 52 years (range 20–75). Diagnoses were non-Hodgkin lymphoma (n=253, 53%), multiple myeloma (MM, 124, 26%), Hodgkin lymphoma (82, 17%), and other hematologic disorders (16, 3%). Forty-seven pts (10%) underwent a second autologous HCT as part of a planned tandem transplantation protocol; readmission and survival were calculated from the time of the first HCT. A total of 193 pts (41%) had a comorbidity score of 0, according to HCT-CI, 146 (31%) had a score of 1 to 2, and 136 (29%) had a score of 3 or greater. The preparative regimens included busulfan, cyclophosphamide, and etoposide (323, 68%), melphalan (86, 18%), and busulfan with cyclophosphamide (66, 14%). The median time to neutrophil recovery was 10 days and to platelet recovery was 14 days. The mean length of hospitalization was 20 +/− 4 days.
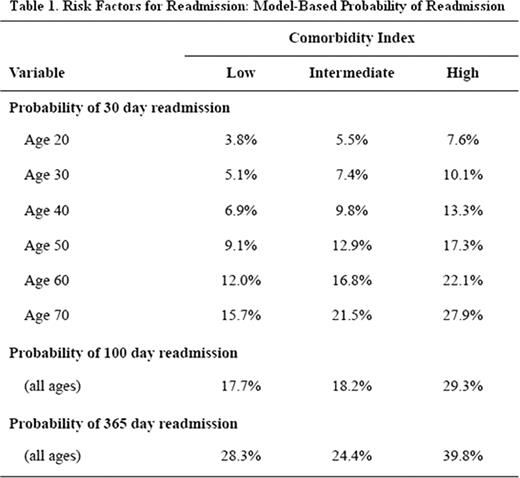
Overall, 14% of patients were readmitted within 30 days of discharge, 21% within 100 days, and 30% within one year. Within the first 30 days post-HCT, infection (62%) and gastrointestinal disorders (22%) accounted for the majority of hospital readmissions. Infection (42%) was also the most frequent reason for readmission within one year, followed by gastrointestinal disorders (16%), relapsed malignancy (14%), and cardiopulmonary disease (9%). By stepwise logistic regression analysis, high pretransplantation HCT-CI (score ≥ 3) was predictive of hospital readmission within 30 days (odds ratio [OR] 2.08, 95% confidence interval [CI] 1.09–3.95, p=.026), 100 days (OR 1.93, 95% CI 1.14.-3.26, p=.014), and one year (OR 1.68, 95% CI 1.04–2.70, p=.034) of HCT discharge. Older age was also prognostic; each ten year increase in age at time of autologous HCT led to an increased likelihood of 30 day readmission (OR 1.36, 95% CI 1.07–1.73, p=.014). A model for probability of post-autologous HCT readmission was constructed using these multivariable risk factors (Table 1).
Cox proportional hazards analysis was used to identify prognostic factors for overall survival. In univariable analysis, high HCT-CI, diagnosis, preparative regimen, and readmission were risk factors for mortality, but in stepwise multivariable analysis, only diagnosis (MM vs other diagnoses, hazard ratio [HR] .61, 95% CI .40-.92, p=.018) and readmission (HR 3.97, 95% CI 2.85–5.52, p<.001) remained prognostic for overall survival.
We conclude that both age and comorbidity status influence readmission rates following autologous HCT. Importantly, readmission is strongly associated with a greater risk of mortality, a link that should be further investigated. HCT-CI scores should be calculated for all autologous HCT pts, which may allow for improved comparison of outcomes and readmission data between institutions and provide opportunities to further increase the safety of autologus HCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal