Abstract
Abstract 907
Most candidates for hematopoietic stem cell transplantation lack a human leukocyte antigen (HLA)-identical sibling donor; however, many patients may have a related donor with whom they are mismatched at one antigen/allele. It is not known whether such a match is preferable to a matched unrelated donor (MUD). We hypothesized that, in transplantation using related donors, adding a single HLA antigen/allele mismatch, identified through high resolution HLA typing at HLA-A, -B, -C, -DRB1 and -DQB1, would be associated with worse outcomes than transplantation using matched unrelated donors.
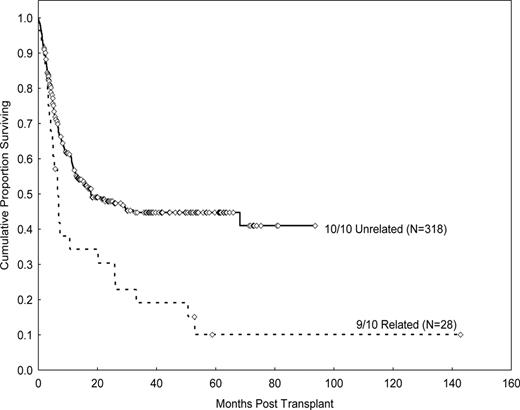
To test this hypothesis, we analyzed outcomes (survival, relapse, non-relapse mortality) of 367 patients who received transplants from either a 10/10 MUD (n=318) or a one-antigen/allele mismatched related donor (MRD) by 7/8 HLA typing (n=49) treated during the same period of time (1995-2009) at our institution. All patients had intermediate/high-resolution HLA typing at all 5 loci either prospectively or retrospectively, if treated after or before year 2002. Of the 49 patients treated with mismatched related donors, 28 patients (57%) had one antigen/allele mismatched at HLA class I or II loci (or 9/10), 18 patients (37%) had 2 alleles mismatched (or 8/10), and 3 patients (6%) had 3 alleles mismatched (or 7/10). From the 28 patients with a one-allele mismatch, 24 had class I mismatches at either HLA-A or -B loci, and 4 had class II mismatches at either HLA-DR or -DQ loci. Characteristics between the MUD group and 9/10 MRD group were similar [median age 53 vs. 47 years (p=0.08); AML/MDS diagnosis 84% vs. 82% (p=0.5); active disease at transplant 59% vs. 57% (p=0.9); myeloablatie conditioning 63% vs. 75% (p=0.2); bone marrow stem cells 58% vs. 70% (p=0.2); pentostatin use 14% vs. 11% (p=0.4); median year of transplant 2006 vs. 2004, respectively] except more patients in the MUD group received ATG (96% vs. 68%, p=0.02).
Outcomes at 3-years were analyzed for the 28 consecutive patients who had received a transplant from a 9/10 MRD based on 5-loci (including -DQB1) HLA typing. Graft failure was more common in patients treated from 9/10 related donors than from MUD. The incidences of primary and secondary graft failure for the 9/10 MRD were 7% and 14%, respectively, whereas none of the MUD transplant recipients had either primary or secondary graft failure (p= 0.02). Cumulative incidence of progression was 40% vs. 25% (p=0.02, HR 1.9, CI 1.1–3.9), non-relapse mortality 40% vs. 26% (p=0.05, HR 1.9, CI 1.0–3.6) and grade II-IV a GVHD was 27% vs. 38% (p=0.4, HR 0.7, CI 0.3–2.5) for the two groups, respectively. Median survival was 6 months for the 9/10 MRD vs. 18 months for the MUD group. The overall survival and progression-free survival rates were 19% and 45% (p=0.007, HR 1.8, CI 1.2–2.9) and 19% vs. 42% (p=0.006, HR1.8, CI 1.2–2.9), respectively. Outcomes for 9/10 MRD transplant patients with class I mismatches (n=24) were significantly worse than outcomes in those with MUD transplants (n=318). The 2-year actuarial OS rate was 27% for the 9/10 MRD and 48% for the MUD transplant group (HR 1.9; 95% CI 1.1 – 3.1; p=0.01).
These results indicate that transplant outcomes for patients treated from a one-antigen/allele mismatch related donor are significantly worse than from a MUD, primarily due to increased non-relapse mortality. Patients receiving transplants form a 9/10 related donors, at least with a class I mismatch, should be treated on investigational protocols.
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal