Abstract
Abstract 901
Many changes have been made to reduce NRM after allo-HCT. While an improvement in NRM has been demonstrated in younger patients who are in remission, NRM has not been examined in other settings, such as in older patients or allo-HCT in non-remission. Therefore, we retrospectively assessed changes in the incidence and causes of NRM over the last 12 years in allo-HCT patients.
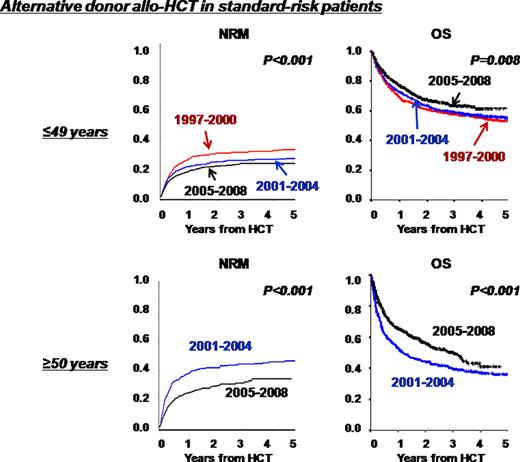
We analyzed a nationwide registry database to estimate the incidence of NRM and overall survival (OS) in patients aged 16 years or older who had acute myeloid leukemia (AML), acute lymphocytic leukemia (ALL) or myelodysplastic syndrome (MDS) and received the first allo-HCT from 1997 to 2008. We compared the NRM incidence after allo-HCT in three consecutive four-year periods (1997-2000, 2001–2004, and 2005–2008) for younger patients (16-49 years), and in the later two periods for older patients (≥50 years). Analyses were separately performed for standard-risk and high-risk patients. The standard-risk group included patients with acute leukemia/MDS in remission or untreated low-risk MDS (RA/RARS), and the high-risk group included those who were not in remission at allo-HCT. Subgroup analyses were performed based on patient age and donor source: HLA-matched/1-Ag mismatched related donor (related donor) versus unrelated bone marrow (BM) or cord blood (CB) donor (alternative donor).
A total of 10003 patients with a median age of 42 years were analyzed and the median follow-up of surviving patients was 37 months (0-154). The proportion of AML, ALL, and MDS patients was 53%, 28%, and 19%, respectively. A total of 2003, 3424, and 4576 allo-HCT were performed in 1997–2000, 2001–2004, and 2005–2008, respectively. The number and proportion of patients aged 50 years or older (n=227, 11%; n=1061, 31%; n=1907, 42%), the use of a reduced-intensity conditioning regimen (n=34, 2%; n=697, 20%; n=1244, 27%) and allo-HCT from an unrelated CB donor (n=42, 2%; n=582, 17%; n=990, 22%) increased over the three periods. An analysis of standard-risk patients (n=6280) showed that the incidence of NRM was 23% at 3 years after allo-HCT. Older patients had a significantly higher NRM than younger patients (31% vs 20%, p<0.001). The donor source significantly affected the incidence of NRM, and unrelated CB had the highest risk of NRM (related, 17%; unrelated BM, 26%; unrelated CB, 32%, p<0.001). The highest incidence of NRM was seen in 2001–2004 (25%) and the lowest incidence was seen in the most recent period, 2005–2008 (22%). A subgroup analysis of younger patients who received allo-HCT from a related donor showed that there was no significant improvement in NRM, and this was 12–15%. In younger patients who received allo-HCT from an alternative donor, the NRM incidence significantly decreased over the three periods (30%, 24%, and 22%, p<0.001) mainly due to a reduced risk of death associated with GVHD, organ failure and lung complications, and OS also significantly improved (58%, 59%, and 64%, p=0.008). In older patients who received allo-HCT from a related donor, NRM significantly improved in 2005–2008 compared to 2001–2004 (29% vs 18%, p<0.001). However, due to the increase in the incidence of relapse in 2005–2008, this decreased NRM did not lead to an improvement of OS (51% vs 55%, p=0.21). In older patients who received allo-HCT from an alternative donor, NRM and OS significantly improved in 2005–2008 compared to 2001–2004 (NRM, 43% vs 31%, p<0.001; OS, 40% vs 51%, p<0.001). The reduction in NRM was mainly due to a significant decrease in death associated with GVHD and infection. In the analysis of high-risk patients (n=3723), the incidence of NRM was generally higher than that in the standard-risk group (34% vs 23% at 3 years, p<0.001). High-risk patients who received allo-HCT from an alternative donor had a significantly lower NRM in the later periods, which led to an improvement in OS. Multivariate analysis indicated that the period of 2005–2008, younger age, and the application of a related donor were independently associated with a lower risk of NRM in both the standard- and high-risk groups.
NRM and OS have recently improved, especially for allo-HCT from unrelated BM or CB donors. These advances were observed not only in younger patients but also in older patients. Although allo-HCT in non-remission was generally associated with a higher risk of NRM, we observed a similar trend regarding the improvement of NRM and OS.
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal