Abstract
Abstract 563
Sonic hedgehog (Shh) is a morphogen regulating epithelial-mesenchymal interactions during embryogenesis. In post-natal life, Shh is a potent indirect angiogenic agent, able to upregulate different families of angiogenic growth factors. Furthermore, Shh gene transfer enhances the contribution of bone marrow (BM)-derived endothelial progenitor cells to myocardial neovascularization. In this study, we tested the beneficial potentials of Shh gene therapy in an experimental model of peripheral limb ischemia, a disease characterized by occlusion of vessels of the arterial circulation of the legs, often secondary to atherosclerosis, thrombosis, and/or inflammatory processes.
Ischemia of the left hindlimb was induced by excising the femoral artery, from its proximal origin as a branch of the external iliac artery till the bifurcation into saphenous and popliteal arteries. Blood flow was measured in ischemic and contralateral hindlimbs by laser Doppler perfusion imaging at days 0, 7, 14, 21, and 28 after ischemia. At day 28, mice were sacrificed and adductor muscles were analyzed for capillary and arteriole density. An additional set of 1-year-old C57BL/6J mice and 8-weeks-old C57BL/6J mice were used to study the effects of Shh gene therapy on mobilization of BM-derived endothelial progenitors in the course of ischemia. Mice were treated with 200 μ g phShh or empty plasmid and hindlimb ischemia was induced 7 days after treatment. Peripheral blood samples were obtained at days 2, 4, and 7 after induction of ischemia. FACS analyses were used to detect cells Lin- and Sca-1+CD34+, Sca-1+CD133+, Sca-1+ Flk-1+, CD14+ Flk-1+, CD14+ CD34+. We also used a BM transplantation model to test the effects of Shh gene therapy on BM-derived cells in the setting of hindlimb ischemia. Wild-type recipient mice received 2×106 BM cells from nls-Ptc1-LacZ mice. Six weeks laster, mice received treatment with 200 μ g phShh or empty plasmid in the hindlimb muscles. Seven days after treatment, ischemia of the left hindlimb was induced. X-gal positive cells were counted on hindlimb muscles 10 days after ischemia. We also measured local expression levels of VEGF165, Ang-1, and SDF-1α proteins in mice treated with 200 μ g phShh or empty plasmid 7 days after ischemia.
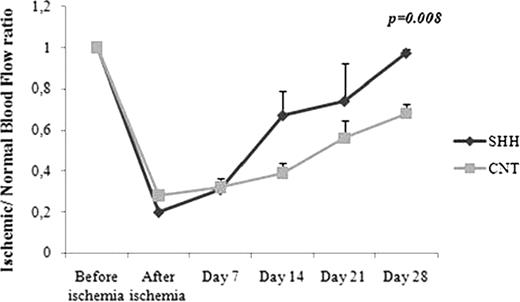
At day 28 after ischemia, blood perfusion ratio between the ischemic and the contralateral leg was 0.97 ± 0.01 in Shh-treated mice and 0.68 ± 0.03 in control animals (p=0.008) (Figure 1a, b). Capillary and arteriole density were significantly higher in the phShh–treated muscles compared to controls (p=0.02; p=0.03, respectively). In both young and middle-aged animals, phShh treatment resulted in significant increase of the number of circulating CD45-/Sca-1+/Flk-1+ and CD45-/Sca-1+/CD133+ cells (p<0.05). In the BM transplantation model, the number of X-gal positive cells in the ischemic site was significantly higher in phShh-treated animals (p=0.000002). Double fluorescent staining for β-gal and BS-1 lectin demonstrated incorporation of these cells into vascular structures, demonstrating that Shh gene therapy increases the number of cells migrating from the BM to the site of ischemia and contributing to the process of neovascularization. Finally, the expression of VEGF, ang-1, and SDF-1α measured after ischemia was significantly higher in animals treated with phShh than in mice treated with control (p= 0.00001; p= 0.00054; p= 0.00003, respectively).
The current standard of care for ischemic diseases of lower extremities relies on direct revascularization, either by endovascular techniques or open surgical approaches. Early preclinical studies and phase I clinical trials achieved promising results with growth factors administered as recombinant proteins or single-agent gene therapies. In this study, we demonstrate that intramuscular administration of a plasmid containing the human Shh gene induces simultaneous activation of angiogenic, arteriogenic, and vasculogenic mechanisms, with beneficial effects in a model of peripheral artery disease. In addition, we showed the ability of Shh gene therapy to increase the number of circulating BM-derived circulating progenitor cells, as well as their incorporation in vascular structures at the level of the ischemic site.
(a) Laser Doppler perfusion imaging. (b) Mice treated with phShh displayed significant increase of the ischemic/contralateral leg perfusion ratio.
(a) Laser Doppler perfusion imaging. (b) Mice treated with phShh displayed significant increase of the ischemic/contralateral leg perfusion ratio.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal