Abstract
Abstract 5068
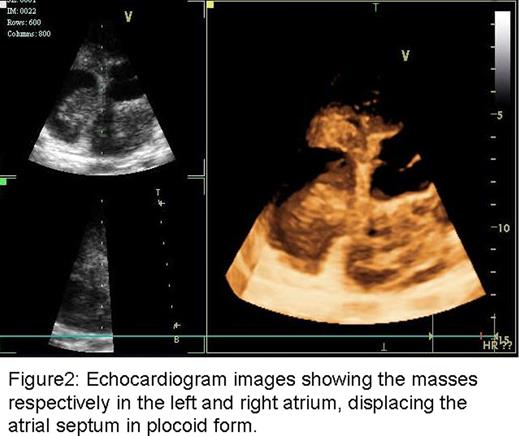
A 33-year-old man of Asian descent was admitted to our hospital 3 years ago with a main complaint of palpitations for 7 months. There was no fever, no cough, no gain or loss of weight, no night sweats, no medical history of allergic diseases or contact with parasites. Physical examination showed marked edema in the neck and upper chest, and the hepatojugular reflux was positive. There was no change in skin appearance or hepatosplenomegaly. A soft rubbery, non-tender lymph node (1×2cm) was palpated in the left axillary area. The laboratory data showed mild eosinophilia (leukocyte count 6000 /ul with eosinophils 582/ul). The serum IgE concentration was increased (1,250 U/ml). Serological tests for HBsAg, anti-HCV, anti-HIV, and antibodies for distoma pulmonala, distoma japonicum, schistosome, bladder worm, sparganum, trichina cystica and filarial were negative, however toxoplasma gondii antibody IgG was positive, while the IgM was negative. Antinuclear antibodies were all negative. Echocardiogram revealed a mass (7.1×7.0×5.5cm) displacing the base of the heart and involving both atria. CT showed enlarged biaxillary lymph nodes and a large mediastinal mass extending into both atria and obstructing the superior vena cava with right ventricular hypertrophy (Fig.1a, b). Positron emission tomography (18F-FDG-PET) scan indicated negative fluorodeoxyglucose (FDG) uptake in the lymph nodes, spleen and liver. Biopsy of an enlarged right axillary lymph node was performed and the pathology revealed a normal preserved nodal architecture with proliferation of lymphoid follicles infiltrated by abundant eosinophils partially forming eosinophilic microabscesses. CD20 staining was positive. The bone marrow examination indicated normal cellularity except a little increase of eosinophils at 7.5%. Biopsy of the cardiac mass was not performed due to technical challenges related to its anatomical location. Based on the clinical and laboratory findings, a diagnosis of Kimura disease was established. Treatment was started with a low dose of oral prednisone 20–30mg/d. After treatment, the enlarged lymph nodes diminished gradually. However, 4 months later, echocardiogram showed the mediastinal mass remained, with two new masses (left 5.4×3.2cm, right 4.3×2.6cm) attached to the atrial septum respectively (Fig2). Prednisone was gradually increased to 50mg/d. 3 months later, the patient was admitted to hospital with chest pain and shortness of breath. Thoracic CT showed severe obstruction of the right middle lobe bronchus by the enlarged mediastinal mass. A bone marrow smear and flow cytometric analysis did not show any clonal hematopoietic abnormality. The echocardiogram remained unchanged. Prednisone (40mg/d) was re-administered but the patient's situation was getting worse quickly. He developed dyspnea and hypoxemia, apparent SVCS, edema of the inferior extremities and recurrent arrhythmia. CHOP chemotherapy was initiated (CTX 1.0 dl, VDS 4mg dl, EPI-ADM 60mg dl, DXM 10mg dl-2) but he died due to cardiac and respiratory failure. Kimura's Disease is a distinct clinicopathological entity accompanied by peripheral blood eosinophilia and elevated serum IgE level. Though rare, KD with cardiovascular involvement has been reported in several cases. This kind of involvement is also named as Eosinophilic Myocarditis (EM), occurs in up to 60% of patients diagnosed with hypereosinophilic syndrome (HES). However, this patient only has partial response of prednisone, and relapsed after 9 months therapy with prednisone 20–50 mg/d. Although chemotherapy was added, it was too late to control the progression of disease. This instructive case demonstrates that although Kimura's disease is a benign process, infiltration of eosinophils in multiple organs may result in critical illness and can be fatal. Early intervention and frequent close followup appears essential for controlling disease in KD patients with cardiac or other critical complications.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal