Abstract
Abstract 4738
High-dose chemotherapy in conjunction with autologous peripheral stem cell transplantation (ASCT) has emerged as a preferred treatment modality for a variety of relapsed hematological malignancies including non-Hodgkin lymphoma (NHL). Failure rates with current mobilization regimens are estimated to be between 5% and 30%. This failure adds substantially to the cost of this already costly procedure due to the need for multiple apheresis sessions following initial mobilization, as well as the implementation of costly rescue protocols. An additional economic burden of this reduced efficacy is increased mortality as fewer patients proceed to transplantation. Plerixafor with G-CSF (G+P) has been shown to be superior to G-CSF (G) alone for stem cell mobilization in heavily pretreated patients with NHL. This increased efficacy reduces the required number of apheresis sessions, reduces the likelihood of rescue, and increases the likelihood of successful engraftment, all of which increases the societal value of plerixafor for this indication. We conducted an economic evaluation of the cost-utility of the G+P as a first line treatment for stem cell mobilization in patients with DLCL versus G alone.
Data from a number of sources were used to construct a decision analytic model to replicate the series of events experienced by a patient undergoing high dose chemotherapy treatment for DLCL, including stem cell mobilization, apheresis, and ASCT. Data from the Washington University site of the plerixafor Phase III study for patients with DLCL (n=20) were used to model the process of stem cell mobilization and apheresis. The probability of mortality post ASCT was taken from the literature. Costs in the model were based upon the Medicare allowable for that service or medication; utilities were taken from the peer reviewed literature. The incremental cost-utility ratio (ICUR) was estimated from a societal perspective with a time horizon of the patient's remaining lifetime using a microsimulation approach.
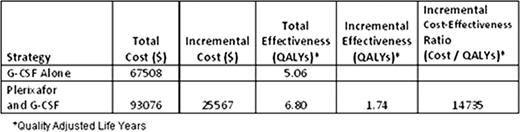
100% (10/10) patients receiving P+G as their first line therapy proceeded to ASCT, while 70% (7/10) of patients receiving G as first line therapy proceeded to ASCT. Patients who did not proceed to transplant were assumed to not contribute any cost or QALYs to the final model result during or after transplant. The expected lifetime cost of providing care for NHL for a person on the P+G treatment was $25,567 more than the G regimen, but they also accumulated 1.74 more quality adjusted life years (QALYs) for an ICUR of $14,735/QALY, due to the greater probability of undergoing transplant. This is well under the willingness to pay of $50,000/QALY accepted in many industrialized nations. In sensitivity analyses we found that this standard of cost-effectiveness was met so long as the probability of transplant was greater than 77%.
The use of plerixafor plus G-CSF for stem cell mobilization in ASCT of patients with DLCL meets most accepted standards of cost-effectiveness. This economic benefit is largely the result of the effectiveness of the P+G regimen in insuring that patients achieve sufficient cell counts to achieve ASCT.
Kymes:Genzyme: Research Funding. Gregory:Genzyme: Research Funding. Lambert:Genzyme: Research Funding. DiPersio:Genzyme: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal