Abstract
Abstract 4562
Analysis of Risk Factors and Outcome for Extramedullary Relapses post Allogeneic Stem Cell Transplantation for Myeloma
Relapse after both autologous and allogeneic hematopietic stem cell transplant (HSCT) is common in multiple myeloma (MM). Unusual sites of relapse have been reported after allogeneic HSCT in the form of isolated extramedullary (EM) lesion or light chain escape. It is hypothesized that these EM relapses are due to changes in the marrow microenvironment or selection of resistant subclones from therapy with novel agents and or allogeneic stem cell transplantation. Several case reports have shown that EM relapse is associated with dismal prognosis compared to medullary or bone marrow (BM) relapse. To study the relapse patterns and outcome, we performed a retrospective analysis of 56 pts who underwent tandem autologous-nonmyeloablative allogeneic HSCT (auto-allo) or reduced intensity conditioning (RIC) allogeneic transplant.
Between January, 2000 to March 2008, 38 pts received planned auto-allo HSCT using melphalan (200 mg/m2) prior to auto-HSCT and TBI (200 cGy) prior to allo-HSCT and 18 pts received RIC allo-HSCT following fludarabine (125mg/m2) and melphalan 140mg/m2. Donors included 52 HLA matched siblings and 4 matched unrelated donors.
Patients characteristics
| Parameters . | Pts without relapse (n) . | BM relapse (n) . | EM relapse (n) . | P-value . |
|---|---|---|---|---|
| Total number of patients | 33 | 16 | 7 | . |
| Age at transplant (median, yr.) | 50.8 | 51 | 54.1 | 0.84 |
| Interval between diagnosis-transplant (median, mo.) | 11.7 | 9.4 | 14.6 | 0.12 |
| B2-micr (median) | 2.06 (1.18-10) | 1.67 (1.28-2.15) | 2.08 (0.79- 9.05) | 0.15 |
| Median f/u for alive pts (yr.) | 6.8 | 8.7 | 9.6 | . |
| Type of transplant | . | . | . | . |
| Auto- allo graft | 70% (23) | 69 % (11) | 57 % (4) | 0.84 |
| RIC | 30% (10) | 31% (5) | 43% (3) | |
| Response before allograft | . | . | . | . |
| CR/PR | 64% (21) | 56% (9) | 71% (5) | 0.79 |
| MR/SD/RE/refractory | 36% (12) | 44% (7) | 29% (2) | |
| Stage III disease at the time of transplant | 78% (25) | 81% (13) | 100% (7) | 0.94 |
| Ch 13 del at dx | 18% (6) | 12% (2) | 29% (2) | 0.69 |
| Novel agent prior to transplant | 45% (15) | 38% (6) | 57% (4) | 0.74 |
| Parameters . | Pts without relapse (n) . | BM relapse (n) . | EM relapse (n) . | P-value . |
|---|---|---|---|---|
| Total number of patients | 33 | 16 | 7 | . |
| Age at transplant (median, yr.) | 50.8 | 51 | 54.1 | 0.84 |
| Interval between diagnosis-transplant (median, mo.) | 11.7 | 9.4 | 14.6 | 0.12 |
| B2-micr (median) | 2.06 (1.18-10) | 1.67 (1.28-2.15) | 2.08 (0.79- 9.05) | 0.15 |
| Median f/u for alive pts (yr.) | 6.8 | 8.7 | 9.6 | . |
| Type of transplant | . | . | . | . |
| Auto- allo graft | 70% (23) | 69 % (11) | 57 % (4) | 0.84 |
| RIC | 30% (10) | 31% (5) | 43% (3) | |
| Response before allograft | . | . | . | . |
| CR/PR | 64% (21) | 56% (9) | 71% (5) | 0.79 |
| MR/SD/RE/refractory | 36% (12) | 44% (7) | 29% (2) | |
| Stage III disease at the time of transplant | 78% (25) | 81% (13) | 100% (7) | 0.94 |
| Ch 13 del at dx | 18% (6) | 12% (2) | 29% (2) | 0.69 |
| Novel agent prior to transplant | 45% (15) | 38% (6) | 57% (4) | 0.74 |
After a median follow up of 7.8 years; there were 16 BM and 7 EM relapses. There was no correlation between either relapse or the pattern of relapse (BM and EM) and development of acute and chronic graft vs. chronic disease (GVHD). The risk ratio for BM relapse in 5 year is 0.27 for patients with chronic GVHD (cGVHD) and 0.15 for patients without cGVHD (P=0.69). The risk ratio for EM relapse in 5 year is 0.12 for patients with cGVHD and 0.25 for patients without cGVHD (P=0.10) (Figure 1).
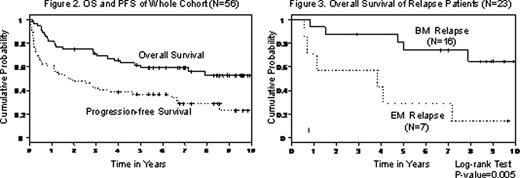
Overall survival (OS) and progression-free survival (PFS) for the whole group (N=56) is shown in figure 1. Four year OS was 43% in EM group and 88% in BM group (P=0.005) (Figure 3).
There were no significant differences between age, B2 microglobulin, numbers of treatment before HSCT, use of novel agents before HSCT, cytogenetics, stage, transplant regimen and development of GVHD and pattern of relapse (BM vs. EM). In conclusion our data suggest that EM relapse can occur post allogeneic HSCT and is associated with shorter overall survival. The development of GVHD does not prevent against EM relapse.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal