Abstract
Abstract 4396
Thromboprophylaxis in women with recurrent pregnancy loss and thrombophilia undergoing fertility treatments: an observational study.
Several phase II studies have suggested a benefit of thromboprophylaxis in pregnant women with histories of recurrent pregnancy loss (RPL) with and without thrombophilia. Two recent phase III studies (ALIFE, SPIN) showed no benefit of thromboprophylaxis in women with RPL, but they were not designed to study women with thrombophilia or with 3 or more miscarriages. In addition, plasminogen activator inhibitor-1 (PAI-1) has been linked to RPL, but there are limited data on the use of thromboprophylaxis in pregnant women with PAI-1 and RPL. A mechanism of unexplained RPL is thought to be placental thrombosis. The patients with thrombophilia who undergo assisted reproduction procedures might be at an increased risk of thrombosis due to multiple gestations, ovarian hyperstimulation and hyperestrogenemia. These could contribute to fetal loss via placental thrombosis. There are limited data on the outcome of pregnant women with histories of RPL treated with assisted reproduction and thromboprophylaxis.
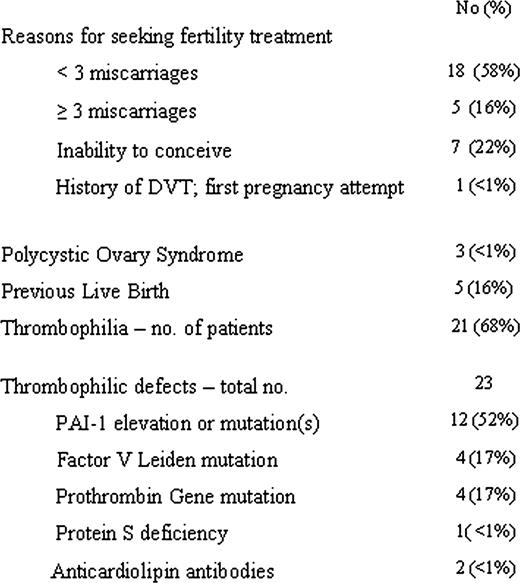
We performed a retrospective review of 31 cases of women of age 20 to 42 that were referred to the Hematology Department at Roosevelt Hospital over the period of five years (between April 2005 and March 2010) for an evaluation prior to undergoing fertility treatment. Aspirin 81 mg daily prior to in vitro fertilization and enoxaparin 40 mg daily upon confirmation of pregnancy or following embryo transfer was recommended for the majority of patients. Aspirin and enoxaparin were recommended for 21 patients; aspirin alone for 5; enoxaparin alone for 4; and no therapy for 1.
Fifteen out of 31 patients took aspirin and enoxaparin; 9, aspirin alone; 4, enoxaparin alone; and 3, no treatment. Sixteen patients had assisted reproduction with in vitro fertilization or intrauterine insemination; 4 received ovulation induction medications; 7 had natural pregnancies; 2 patients had pregnancies by unknown means.
Twenty-five patients (81%) conceived; 13 (42%) had term deliveries; and 1(<1%) had a pre-term delivery at 31 weeks. Five patients (16%) were pregnant at last follow-up. Seven patients (22%) miscarried. Six patients (19%) did not conceive.
Thromboprophylaxis was associated with a high pregnancy rate and a high live birth rate in women with RPL, many with thrombophilia including PAI-1, presenting for fertility treatment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal