Abstract
Abstract 4276
To date, the efficacy of various iron chelators in reducing cardiac iron, a leading cause of death in transfused patients with β-thalassemia major (TM), has been demonstrated in prospective controlled studies of up to 1-yr duration. Since removal of iron from the heart takes several years, it is important to assess longer-term effects of iron chelation therapy in terms of cardiac iron removal. We report here end-of-study (EOS) results from the EPIC cardiac substudy in TM patients treated with deferasirox for up to 3 yrs.
Patients aged ≥10 yrs with myocardial T2* >5 to <20 ms (indicating cardiac siderosis) by cardiovascular magnetic resonance (MR), left ventricular ejection fraction (LVEF) ≥56%, serum ferritin >2500 ng/mL, MR (R2) liver iron concentration (LIC) >10 mg Fe/g dry weight (dw) and ≥50 lifetime transfused blood units were included in the study. Deferasirox was initiated at 30 mg/kg/day and increased to 40 mg/kg/day by the start of yr 2. Dose decreases were allowed for safety reasons. Primary endpoint was change in myocardial T2* from baseline (BL) to 3 yrs.
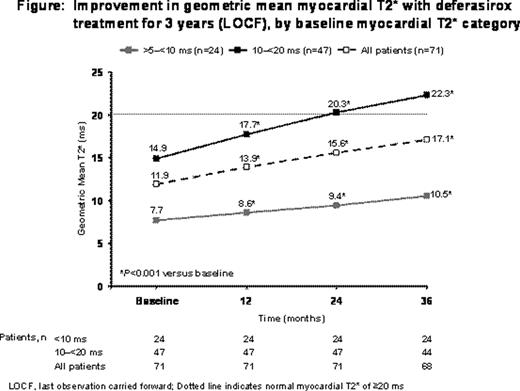
Seventy-one patients completed 2 yrs of treatment and entered the 3rd yr of the study. Mean age was 20.5 ± 7.4 yrs. BL cardiac T2* was >5 to <10 ms (severe cardiac siderosis) in 24 patients (34%) and 10 to <20 ms (moderate-to-mild cardiac siderosis) in 47 patients (66%). All patients were previously chelated with deferoxamine (DFO) or DFO and deferiprone. Mean actual deferasirox dose was 33.3 ± 3.9, 35.4 ± 8.0 and 33.6 ± 9.8 mg/kg/day during the 1st, 2nd and 3rd yr, respectively. Geometric mean T2* significantly increased from 11.9 ms ± 39.0% at BL to 13.9 ms ± 46.9% after 1 yr, 15.6 ms ± 57.7% after 2 yrs, and continued to increase to 17.1 ms ± 62.0% after 3 yrs, (increase from BL of 17% at 1 yr, 31% at 2 yrs and 44% at 3 yrs; P<0.001 vs BL at each yr; Figure). In patients with BL T2* 10 to <20 ms, geometric mean T2* increased significantly to normal levels (≥20 ms) by 2 yrs and further increased to 22.3 ms ± 48.8% at EOS (36% and 50% increase from BL, respectively). Those with BL T2* >5 to <10 ms also showed significant increases; geometric mean T2* reached near moderate-to-mild severity (9.4 ms ± 31.5%) by 2 yrs and continued to increase to 10.5 ms ± 42.5% at EOS (22% and 36% increase from BL, respectively).
After 3 yrs, 68.1% of patients with BL T2* 10 to <20 ms normalized to ≥20 ms; 50.0% of patients with BL T2* >5 to <10 ms improved to 10 to <20 ms. LVEF was stable in the normal range over 3 yrs. Mean LIC significantly reduced from 28.4 ± 9.7 mg Fe/g dw at BL to 15.5 ± 14.1 mg Fe/g dw at EOS (–47%; P<0.001). Median serum ferritin also significantly reduced from 5575 ng/mL at BL to 2794 ng/mL at EOS (–46%; P<0.001).
Of 71 patients, 66 (93.0%) completed the 3rd yr. Reasons for discontinuation were unsatisfactory therapeutic effect (n=3) and consent withdrawal (n=2). There were no deaths during the 3-yr study. Drug-related AEs (≥5%) decreased year by year: increased blood creatinine (n=19 [26.8%] vs n=16 [22.5%] vs n=9 [12.7%]), rash (n=11 [15.5%] vs n=0 vs n=0), increased ALT (n=5 [7.0%] vs n=3 [4.2%] vs n=2 [2.8%]), increased AST (n=4 [5.6%] vs n=3 [4.2%] vs n=1 [1.4%]) and diarrhea (n=4 [5.6%] vs n=1 [1.4%] vs n=0). In yr 3, serious AEs included atrial fibrillation, chronic sinusitis, femur fracture, gastritis, muscle abscess and rheumatic fever (all n=1); none were considered deferasirox-related. Six patients (8.5%) had 2 consecutive increases in serum creatinine >33% above BL and upper limit of normal (ULN); 3 patients in the 1st yr and 3 in the 3rd yr. Two (2.8%) patients had 2 consecutive increases in ALT >10 × ULN; 1 patient in the 2nd yr and 1 patient in both the 2nd and 3rd yr.
This is the first prospective study to report 3-yr data on cardiac iron removal for an iron chelator. Once-daily deferasirox monotherapy at doses of 30–40 mg/kg/day effectively removed cardiac iron, allowing 68% of patients with moderate-to-mild cardiac iron loading to normalize and 50% of patients with severe myocardial iron loading at BL to reduce their cardiac iron levels to the moderate-to-mild range, associated with a much lower risk of heart failure. Importantly, there were no reports of death during the study. The long-term improvements in cardiac iron loading with deferasirox at doses of >30 mg/kg/day were associated with a manageable safety profile, maintenance of normal cardiac function and a concomitant significant decrease in hepatic and total body iron burden by nearly 50% over the 3 yrs.
Pennell:Siemens: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Apotex: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; CVIS: Equity Ownership. Porter:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Cappellini:Novartis: Speakers Bureau. Aydinok:Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Ibrahim:Novartis: Honoraria. Li:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees. Viprakasit:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Kattamis:Novartis: Honoraria, Research Funding, Speakers Bureau. Smith:Novartis: Consultancy, Research Funding. Habr:Novartis: Employment. Domokos:Novartis: Employment. Roubert:Novartis: Employment. Taher:Novartis: Honoraria, Research Funding.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal