Abstract
Abstract 4149
Follicular lymphoma (FL) is the second most common type of lymphoma in Europe and North America. Traditionally, FL has been graded according to the number of centroblasts in the follicles per high power field, to grades 1–3. This grading system, however, does not capture the clinical variability observed in low grade (1-2) FL. The recent WHO classification made it clear that clinically, FL grade 1 and 2 cannot be distinguished, with generally long median survival and recurrent relapses, while grade 3 FL generally has a more aggressive course. Though the clinical prognostic indices such as the FLIPI and the IPI can provide information regarding outcome, they fail to define the biology of the disease. Proliferation index (PI) as determined by Ki-67 immunohistochemistry (MIB-1) has been shown by some to have prognostic value in FL, while others did not find any significance. The PI value in FL is usually determined either by counting cells or by visual estimation. We previously validated the use of quantitative image analysis (QIA) in mantle cell lymphoma, and showed that it is a robust tool for determination of the PI. It is objective and highly reproducible. In this study we aim to evaluate the prognostic significance of PI in a retrospective cohort of pts with FL, grade 1–2.
Specimens from 73 FL pts (33 man, 40 women) diagnosed between the years 2001–2008 were identified. Clinical data was obtained by thorough chart review. All specimens were reviewed by an experienced hematopathologist and the grade confirmed. There were 59 grade 1–2 and 14 grade 3 cases. Slides were scanned with the ScanScopeXT (Aperio, Vista, CA) using brightfield imaging at 200x magnification. Follicles were annotated using ImageScope (Aperio) and analyzed using Aperio image analysis software. Inter-follicular areas were not analyzed. Survival analysis was done by the Kaplan-Meier method. Differences between groups were analyzed using chi-square test and Fisher's exact test.
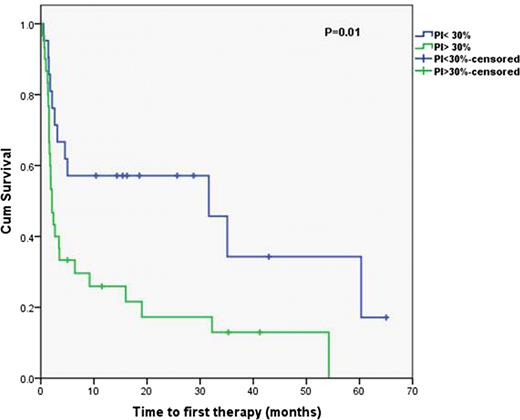
Median age at diagnosis was 61.8 years. Median follow-up time for all 73 pts was 38.8 m (range 0.95 to 102.3). The median PI for the entire group was 33%. When analyzing grade 1 and 2 separately (no=59), the median was almost the same (32%) (Fig 1). We found no significant correlation between grade and PI in this cohort. Outcome for pts with grade 1–2 disease was analyzed by dividing the pts based on PI: low PI (PI<30%); and high PI group (PI>=30%). These two groups did not differ in clinical characteristics including: age, clinical stage, FLIPI score, or the indication for first treatment. Overall survival (OS) (median not reached) and event-free survival (EFS) (median 54.2 m) were not statistically different between the groups. However, time to first therapy (TTFT), was significantly shorter for the high PI group (p=0.01) (Fig 2). The median time to first therapy for FL, grade 1–2, was 3.4 m. Within this group, the time to first treatment was 2.1 m v 31.6 m, for the high and low PI groups, respectively. As the curves indicate, the difference between the groups starts approximately 3–6 months after diagnosis. A similar analysis of FLIPI risk group (low and intermediate v high) failed to demonstrated differences in OS, EFS and TTFT.
We conclude that PI varies significantly among low grade FL pts. This variability may relate to the clinical course of these pts. We have shown significantly different time to first therapy between the low and high PI groups. We plan to further explore differences in OS and EFS in a larger series of FL pts and confirm the predictive value of PI for TTFT.
PI distribution as determined by QIA among all cases of FL.
Time to first therapy for low grade FL pts separated to low and high PI.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal