Abstract
Abstract 4048
The plasma cell labeling index (PCLI) is measured as the percentage of bone marrow plasma cells (PC) in the S phase of the cell cycle and provides an estimate of the proliferative capacity of malignant PC in multiple myeloma (MM). The International Myeloma Working Group (IMWG) uniform response criteria measure the monoclonal (M) protein and serum free light chain (FLC) assay to evaluate clinical response. An elevated PCLI is an established adverse prognostic risk factor for survival, however it is unknown if the PCLI response to therapy offers further prognostic value.
Data from 176 newly diagnosed MM patients from 1985 to 2005 were collected from the Mayo Clinic dysproteinemia database. Inclusion criteria for the study required a minimum initial PCLI of 0.5% and a subsequent PCLI 4 months after initiation of therapy. Baseline and subsequent serum M-protein, progression date, and overall survival were recorded. Clinical responses were assessed by the IMWG uniform response criteria. The association of PCLI response and treatment response (CR, VGPR, or PR) was assessed univariately. Overall survival based on PCLI response, M-spike reduction, and treatment response by IMWG criteria was estimated using the Kaplan-Meier method.
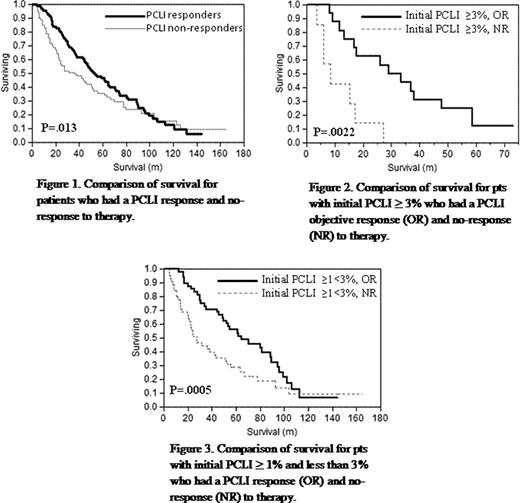
The median overall survival (OS) was 47 months (range: 4 – 165). Ninety-four patients (53%) demonstrated a ≥60% reduction in PCLI after initial therapy (responders) and this conferred a significant OS advantage of 51 months vs. 34 months (P<0.01; Figure 1) compared to those who achieved <60% PCLI reduction (non-responders) after initial therapy. The median PCLI percent difference following 4 months of therapy was -67% (+/− 137%; range: -100 to 953%). When patients were stratified into high (PCLI of ≥3%), intermediate (PCLI ≥1%) and low (PCLI <1%) risk groups, OS was significantly improved in the high and intermediate PCLI groups if they achieved ≥60% reduction in PCLI after initial therapy, 31 vs. 7 months (P<0.0022; Figure 2) and 63 vs. 25 months (P<0.0005; Figure 3), respectively. As observed in prior studies, patients with PCLI of ≥3% at diagnosis had shorter overall survival (17 months) when compared to patients with an initial PCLI of <1% (61 months; P < 0.0001). Of the 94 responders, 39% (n=37) did not achieve a response to therapy as measured by M-protein. Thirteen patients (14%) had no measurable serum M-protein at baseline. Conversely, 35% (n=31) of patients that responded by M-protein criteria did not achieve a PCLI response. In patients who achieved CR/PR after 4 months of therapy, the median PCLI reduction was 83.7% vs. 22.5% (P <0.0004) compared to patients with stable disease (not meeting criteria for CR or PR) or progressive disease (as specified by IMWG response criteria). This reflects a significant reduction in disease burden and as expected, median OS was better in the CR/PR group (53 vs. 31 months, P <0.0016).
Our study demonstrates that the degree of PCLI reduction after therapy is important in predicting overall survival and response to therapy. This is an important finding in the current setting of effective MM treatment options, whereby patients who do not achieve an adequate response as defined as ≥60% reduction in PCLI in our study, may require change in therapy. Our data confirm that reduction of M-protein is an important surrogate endpoint, as patients who achieved PR and CR lived significantly longer. A significant portion of individuals 39% had a measurable response by PCLI that was not detected by M-protein. Further studies are needed to evaluate the predictive value of the addition a criterion that looks at reduction in proliferative rate as measured by PCLI or other methods such as flow cytometry.
Greipp:Mayo Clinic: Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal