Abstract
Abstract 3888
A lower incidence of Hodgkin's lymphoma (HL) in Asians has been recognized and the incidence of HL in Korea was reported to be 5.3%. This low incidence of HL in Asian population has hindered the evaluation of pathogenesis and prognostic factors of the disease. Although international prognostic score (IPS) has been largely utilized as prognostic stratification tool, there has been unmet need to further clarify those with poor prognosis until an increased number of tumor-associated macrophages was identified as a predictor of poor clinical outcome. Hence, we evaluated the prognostic significance of CD68, a marker of macrophages, in Korean HL patients.
We performed immunohistochemical analysis of CD68 in 144 classic HL patients treated with ABVD (n=113, 78.5%), MOPP (n=10, 6.9%), ABVD/MOPP hybrid (n=15, 10.4%) or BEACOPP (n=6, 4.2%) chemotherapy with or without radiotherapy between November 1990 and December 2009 in the Asan Medical Center. The relative percentage of CD68+ cells in relation to overall cellularity was calculated and the results were correlated with clinical outcome.
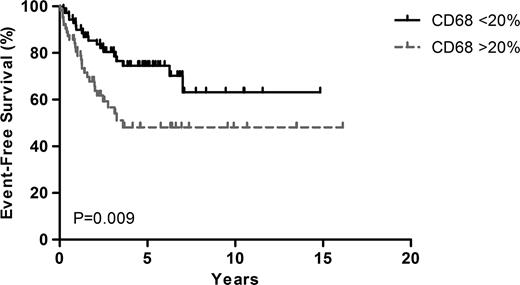
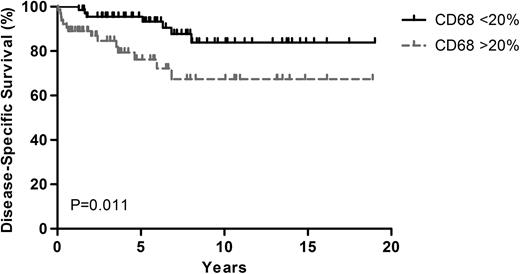
We examined various cutoff points of CD68 expression from 10 to 90 percentile with a rising gradient constructed using 5% steps (5%, 10%, 15%, 20%, 25%, 30%, 35% and 40%). The most significant statistical difference in disease-specific survival (DSS) was observed at a cutoff value of 20%, employing the log-rank test. The high (>=20%, n=78) CD68 group included more patients with older patients (Age 45 yr, 45.5% vs. 28.2%, p=0.032) and higher IPS (>=4, 37.9% vs. 21.8%, p=0.034) compared with the low (<20%, n=66) CD68 group. In total, 18 patients in the low CD68 group and 20 patients in the high CD68 group experienced relapse or progression. Nine patients in the low CD68 group (6 patients of progressive disease [PD], 1 of treatment-related infection during salvage treatment, 1 of moyamoya disease and 1 of unknown cause) and 15 patients in the high CD68 group (8 of PD, 5 of treatment-related infection, 1 of intraventricular hemorrhage during primary therapy, 1 of unknown cause) died by the time of data cutoff. Treatment-related mortality (TRM) was significantly higher in the high CD68 group (n=1 vs. n=6, p=0.048). The 5-year EFS rates were 74.7% and 49.5% in the low and high CD68 expression groups, respectively (P=0.009) with a median follow-up period of 5.4 years (range, 0.6–19.0 years) in surviving patients. The 5-year DSS rates were 95.7% in the low CD68 expression group and 76.5% in the high CD68 expression group (P=0.011). In the multivariate analysis with clinical variables significantly correlating with EFS/DSS in univariate analyses including IPS (>=4), age (>=45 years) and presence of B symptoms, CD68 expression was found to be an independent prognostic factor for EFS (Hazard ratio [HR] =1.846; 95% confidence interval [CI] 1.106–3.354; P=0.044) and DSS (HR = 2.955; 95% CI, 1.148–7.607; p=0.025). However, the prognostic significance of CD68 seems to be more prominent in patients with localized disease (n=48) in a subgroup analysis. While 5-year EFS (85.8% vs. 25.7%, p=0.001) and DSS (95.7% vs. 78.8%, p=0.007) for patients with localized disease were significantly higher in the low CD68 group, both EFS (66.5% vs. 56.5%, p=0.144) and DSS (92.7% vs. 75.7%, p=0.144) were not significantly different between the high and low CD68 groups.
The number of CD68+ macrophages is a significant prognostic factor in Korean HL patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal