Abstract
Abstract 3569
High dose therapy (tx) with autologous hematopoietic stem cell transplantation (AHSCT) in (rel/rfr) lymphoma is the standard of care in the general population with chemosensitive disease. The feasibility of second line therapies (Tx) and AHSCT in (rel/rfr) AIDS related lymphoma (ARL) has been shown in a number of trials. However, the true impact of 2nd line tx and AHSCT is unknown, as nearly all studies focus on those already with disease sensitive to 2nd therapy going onto transplantation. The only recent study capturing patients (n=50) before 2nd line tx showed 49% progression-free survival (Re et al. Blood 2009). Here, we retrospectively analyzed the outcome of patients (pts) presenting at 13 US AIDS Malignancy Consortium sites with (rel/rfr) ARL in the HAART era.
HIV-positive pts initiating tx for (rel/rfr) ARL between 1997–2008 were included. Overall survival (OS) was calculated from the initiation of 2nd line tx.
A total of 126 pts received 2nd line tx. Only those 88 pts who received 2nd line with curative intent to treat (ITT) were included in the analysis. Baseline and selected clinical characteristics are summarized in the table. Median CD4 at HIV diagnosis was 110 (n=37) with a range of 12 to 1000. At ARL dx, median CD4 was 152 (5-803). 47% had an opportunistic infection (OI) prior to ARL. 2nd line tx were: ICE (n=34), EPOCH (n=16), ESHAP (n=11), High-dose MTX variants (n=10), Hodgkin's specific tx (n=5), DHAP (n=4) and others (n=8). Thirty-two (36%) had a response to 2nd line tx (CR, n=21; PR, n=11). Of 50 pts with grade ≥3 toxicities, the most common were thrombocytopenia (46%) and neutropenic fever (44%). Six pts died during 2nd line tx due to infectious complications, with 1 aspergillosis.
Best response to 2nd line tx:
| . | All=88 (%) . | AHSCT=16 (%) . | Non-AHSCT=72 (%) . |
|---|---|---|---|
| CR | 21 (24) | 5 (31) | 16 (22) |
| PR | 11 (13) | 5 (31) | 6 (8) |
| Stable | 7 (8) | 4 (25) | 3 (4) |
| Refractory | 49 (56) | 2 (13) | 47 (65) |
| . | All=88 (%) . | AHSCT=16 (%) . | Non-AHSCT=72 (%) . |
|---|---|---|---|
| CR | 21 (24) | 5 (31) | 16 (22) |
| PR | 11 (13) | 5 (31) | 6 (8) |
| Stable | 7 (8) | 4 (25) | 3 (4) |
| Refractory | 49 (56) | 2 (13) | 47 (65) |
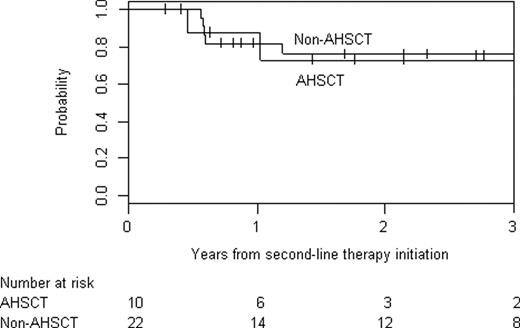
Thus, CR/PR was 32/88 (36%) in ITT analysis. Only 10/32 CR/PR pts went onto AHSCT due to availability and changing treatment paradigms. Conditioning was BEAM (n=9) and Bu/Cy (n=7). No pt went onto allotransplant. At AHSCT day +90, 10 pts were in CR. For all pts, median follow-up was 122 weeks (range, 8–597), median OS was 38 weeks (95% CI, 27–63). Reflecting the 65% prevalence of pts refractory to 2nd line tx in the non-AHSCT group, OS was longer in pts who underwent AHSCT compared to those who did not (2-year OS: 55.3% vs. 31.0%). Surprisingly, 1-year OS in the CR/PR pts was 87.5±12.5% for AHSCT and 81.8±8.2% for non-AHSCT. One Burkitt pt survived a year without AHSCT. Discussion: Rel/rfr ARL was treated aggressively in this largest ever reported cohort, but CR/PR was only 32/88 (36%) in ITT analysis. Not all CR/PR pts went onto AHSCT due to changing treatment paradigms and regional availability. Aggressive 2nd line tx and ASHCT was feasible despite prior low CD4 and OI, but DFS may be possible without transplant. We cannot draw conclusions about the impact of AHSCT from this retrospective cohort. Similarly, it is not known whether survival in (rel/rfr) ARLs is equivalent to the HIV negative population. The current paradigm is to offer pts with rel/rfr ARLs AHSCT if disease is chemosensitive and no contraindication exist. New strategies are needed for 2nd line therapy, particularly in rel/rfr BL.
| Characteristics . | Overall (N=88) . | AHSCT (n= 16) . | Non-AHSCT (n=72) . |
|---|---|---|---|
| Age at study entry (yrs) * | 42 (21–61) | 44 (32–61) | 42 (21–59) |
| Primary refractory | 54 (61%) | 6 (38%) | 48 (67%) |
| CD4 * (n=80) | 172 (5, 803) | 154 (12,653) | 180 (5,803) |
| ECOG PS <=2 | 84 (95%) | 16 (16%) | 68 (94%) |
| Pathology | |||
| DLBCL | 49 (56%) | 5 (31%) | 44 (61%) |
| BL +variants | 12 (14%) | 0 | 12 (17%) |
| PBL | 5 (6%) | 2 (13%) | 3 (4%) |
| HL | 10 (11%) | 5 (31%) | 5 (7%) |
| T cell lymphomas | 4 (5%) | 2 (13%) | 2 (3%) |
| Other | 8 (9%) | 2 (12%) | 6 (7%) |
| Extranodal involvement | 22 (25%) | 6 (38%) | 16 (22%) |
| N of extranodal sites * (n=21) | 1 (0,4) | 1 (0,3) | 1 (0,4) |
| OS (±SE) at 2 years post- 2nd line tx † | 35.4 ± 5.7% | 55.3 ± 13.7% | 31.0 ± 6.1% |
| OS (±SE) at 1 years post- 2nd tx for CR/PR pt† | 83.3 ± 16.7% | 87.5 ± 12.5% | 81.8 ± 8.2% |
| Characteristics . | Overall (N=88) . | AHSCT (n= 16) . | Non-AHSCT (n=72) . |
|---|---|---|---|
| Age at study entry (yrs) * | 42 (21–61) | 44 (32–61) | 42 (21–59) |
| Primary refractory | 54 (61%) | 6 (38%) | 48 (67%) |
| CD4 * (n=80) | 172 (5, 803) | 154 (12,653) | 180 (5,803) |
| ECOG PS <=2 | 84 (95%) | 16 (16%) | 68 (94%) |
| Pathology | |||
| DLBCL | 49 (56%) | 5 (31%) | 44 (61%) |
| BL +variants | 12 (14%) | 0 | 12 (17%) |
| PBL | 5 (6%) | 2 (13%) | 3 (4%) |
| HL | 10 (11%) | 5 (31%) | 5 (7%) |
| T cell lymphomas | 4 (5%) | 2 (13%) | 2 (3%) |
| Other | 8 (9%) | 2 (12%) | 6 (7%) |
| Extranodal involvement | 22 (25%) | 6 (38%) | 16 (22%) |
| N of extranodal sites * (n=21) | 1 (0,4) | 1 (0,3) | 1 (0,4) |
| OS (±SE) at 2 years post- 2nd line tx † | 35.4 ± 5.7% | 55.3 ± 13.7% | 31.0 ± 6.1% |
| OS (±SE) at 1 years post- 2nd tx for CR/PR pt† | 83.3 ± 16.7% | 87.5 ± 12.5% | 81.8 ± 8.2% |
PS: Performance status, DLBCL: Diffuse large B-cell lymphoma, BL: Burkitt or Burkitt-like lymphoma, PBL: Plasmablastic lymphoma, HL: Hodgkin's lymphoma, OS: Overall survival.
Median (range),
Median (95% confidence interval).
OS in CR/PR pts by transplant:
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal