Abstract
Abstract 3510
The outcome in FL pts relapsing after ASCT has not been well studied. While the use of nonmyeloablative allogeneic stem cell transplantation (NST) has been promising in this setting, one could not underestimate the results of selective inclusion criteria.
All patients with FL who experienced a relapse after ASCT at The University of Texas M. D. Anderson Cancer Center between 1997 (the initiation of the rituximab and NST era) and 2007, were analyzed.
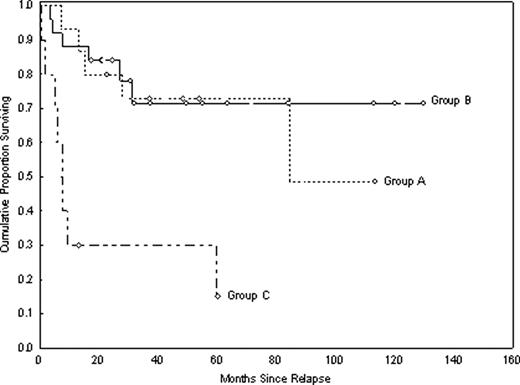
Fifty pts were identified. Fifteen (30%) pts underwent NST after ASCT relapse (Group A); 25 (50%) pts (Group B) met the eligibility criteria for NST but were not allotransplanted due to either physician/pt preference (n=14), lack of suitable donors (n=5), insurance requirements (n= 3), other causes (n=3). Ten (20%) pts (Group C) were not eligible for NST due to refractory disease or co-morbidities. At the time of progression after ASCT, the comparison of pts who were considered for NST showed that Group A pts and Group B pts had a comparable age [median 57 years(range, 45–64) vs 58 years (range, 40–70), p=0.7, respectively], serum LDH level (p=0.1), # of extranodal sites of disease (p=0.4), marrow involvement (p=0.1), and stage III/IV (p=0.2). The histology subtypes were also equally distributed in both groups (FL grades 1, 2, and 3 were found in 27%, 40% and 30% of Group A pts, respectively, and in 16%, 44% and 40% of Group B pts, respectively). The majority of pts in Groups A and B had a good ECOG PS of 0–1 (100% vs 96%, respectively). The median time from ASCT to progression was 16 months (range, 4–42) in Group A, and 19 months (range, 3–99) in Group B. Group A pts underwent their NST at a median of 8 months after their ASCT relapse. At their progression post ASCT, pts in Group B were treated with either rituximab as a single agent (n=12, 48%), or combination chemo-antibodies (n=7, 28%); the therapy received in the remaining 6 (24%) pts was unknown. With a median follow-up time of 49 months (range 23–113 months) for Group A, and 37 months (range, 17–130 months) for Group B, the actuarial survival rates at 4-year were 73%(%95 CI, 42–89) and 71% (%95 CI, 46–86), respectively, (Figure, p = 0.9). The causes of death in Group A were related to infection (1), organ failure (1), progression (2), and unknown (1). Five pts in Group B died of progression and one died of secondary leukemia. Pts in Group C had a median survival time of 7 months; only 2 pts of this group were still alive at the time of this analysis was made.
Single institution results show that 30% of pts with FL relapsing after ASCT undertook an allotransplant. While allogeneic NST is an effective therapy for these pts, a significant proportion of pts can be observed for several years before an allotransplant should be considered.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal