Abstract
Abstract 322
anaplastic large-cell lymphoma (ALCL) is a T-cell lymphoma characterized by peculiar morphologic features and strong expression of CD30. Based on the anaplastic lymphoma kinase (ALK) protein expression, the current WHO classification distinguishes ALK+ and ALK- systemic ALCL as separate disease entities. ALK+ ALCL has classically a better prognosis than ALK- ALCL, however the independant prognostic value of ALK expression remains debated and the long term outcome of adults with systemic ALCL is not known.
eligibility criteria for this study included patients with confirmed diagnosis of systemic ALCL after immunohistopathological review and defined ALK expression status. Patients were retrieved from the GELA LNH87-LNH93-LNH98 prospective clinical trials. Most patients received an anthracyline-based regimen as first line treatment.
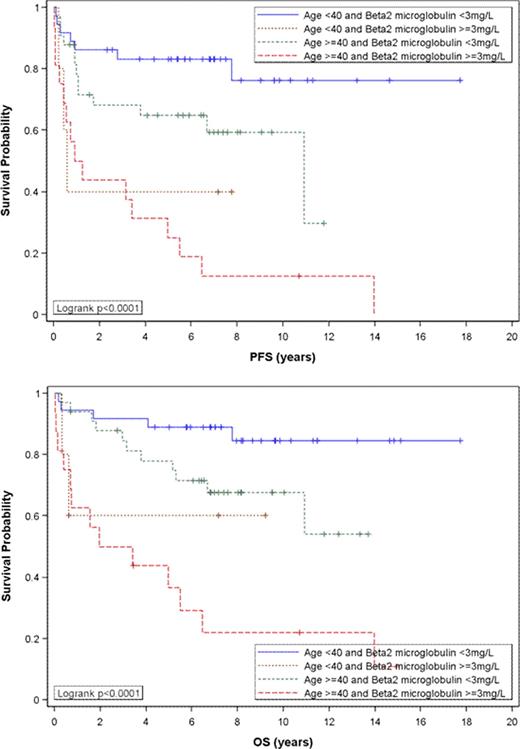
of the 138 included patients with systemic ALCL, 64 (46%) were ALK+ and 74 (54%) were ALK-. The median follow-up duration was 8 years. At diagnosis patients with ALK+ ALCL were younger than those with ALK- ALCL (median age 31 vs 56 years) with significantly more patients < 40 years in ALK+ group (66% vs 23%, p<0.0001). There was a predominance of males in both types (64%). The performance status (PS) was poor (≥2) in 16% (ALK+) vs 33% (ALK-) (p=0.019). The IPI score was high (3-5) in 24% (ALK+) vs 48% (ALK-) (p=0.03). Beta2microglobulin (level available in 90/138 patients) was ≥ 3 mg/L in 12% (ALK+) vs 33% (ALK-) (p=0.016). Ann Arbor stage, elevated LDH, number of extranodal sites > 1, bulky disease (mass > 10 cm), B symptoms, blood cell counts, hypoalbuminemia < 35 g/L and gammaglobulin level had a similar distribution in ALK+ and ALK- patients. The overall response rate to first line treatment was better in ALK+ than in ALK- patients (89% vs 76%, p=0.0417). Eleven patients died during first line treatment, all in the ALK- group. All these patients had disseminated disease. Fourteen (22%) patients relapsed in ALK+ group vs 26 (35%) patients in ALK- group. After 3 years, there was no relapse in ALK+ group, whereas 3/26 relapses in ALK- group (2 relapses after 5 years). The 8-year progression-free survival (PFS) was 54% (95% CI 45–63%) for the entire cohort, 72% (95% CI 58–83%) in ALK+ vs 39% (95% CI 27–51%) in ALK- patients (p=0.0005), and 8-year overall survival (OS) was 64% (95% CI 55–72%) for the entire cohort, 82% (95% CI 69–89%) in ALK+ vs 49% (95% CI 37–61%) (p<0.0001). Clinical and laboratory features were tested in univariate analysis for their impact on PFS and OS in the whole cohort and in ALK+ and ALK- groups. IPI (and its 5 factors taken individually), age < 40 years, ALK status, mediastinal, lung, liver and spleen involvement, hypoalbuminemia < 35 g/L and beta2microglobulin ≥ 3 mg/L had a significant impact on PFS and OS. Interestingly, in patients < 40 years old, there was no impact of ALK status on PFS/OS. In multivariate analysis taking into account factors of IPI (with a cut-off at 40 years for age) and ALK status, only number of extranodal sites, age and ALK status remained significant predictors of PFS and OS. Adding beta2microglobulin to these 6 factors resulted in a model in which only beta2microglobulin (p= 0.0003 for PFS and p=0.0004 for OS) and age (p= 0.04 for PFS and p=0.03 for OS) had a significant impact on PFS and OS, beta2microglobulin being the most discriminant factor (Figure). Not all the ALK- ALCL had a poor prognosis, and reciprocally not all the ALK+ ALCL had a favorable outcome.
this long term study of ALCL emphasizes the prominent impact of age and beta2microglobulin both in ALK+ and ALK- ALCL in PFS and OS. These two factors could be useful for improving the prognostic assessment of patients with ALCL. They could also be of help in stratifying patients in prospective trials.
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal