Abstract
Abstract 3215
Anemia is a common condition among older adults associated with substantial morbidity and mortality. Previous studies indicate that no discernible etiology (i.e., UAE) occurs in around 1/3rd of elderly anemia pts. Limited data exist regarding prospective and careful evaluation to establish the full spectrum and incidence of the diverse etiologies of anemia in the elderly. In addition, minimal data are available for non-white populations.
We prospectively studied 174 subjects 65 yrs and older referred to the University of Chicago Hematology Clinic primarily for evaluation of anemia defined by hemoglobin (Hb) < 13.0 g/dL and < 12.0 g/dL for men and women, respectively. An extensive standardized history, physical and laboratory evaluation ensued with bone marrow (BM) evaluation as indicated. A diagnostic algorithm was applied for anemia categorization with specific criteria, which included a designation of iron deficiency anemia (IDA) for a serum ferritin < 50 ng/mL or lack of erythroid response after iron repletion. Chronic kidney disease (CKD) related anemia required an estimated GFR of < 30 mL/min/1.73m2 applying the four-variable Modification of Diet and Renal Disease (MDRD) study group criteria.
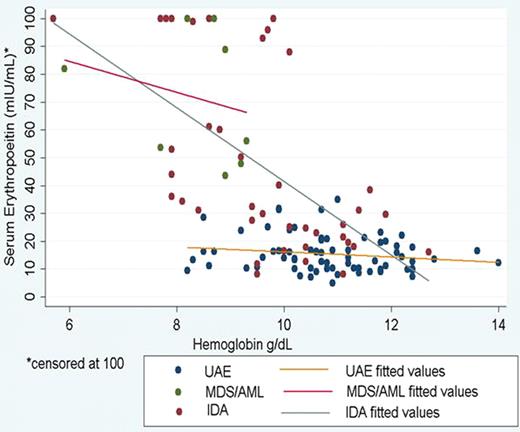
Median age was 76 yrs and 60.3% of pts were female. African-Americans (AA) accounted for 69% of pts and whites were 27%. Hypertension and diabetes were frequent at 79% and 39%, respectively. The median hemoglobin (Hb) was 10.2 g/dL and mean MCV of 88. Approximately 17% of pts had received red blood cell (RBC) transfusion in the prior 3 months. Median eGFR was 61.5. C-reactive protein was ' 3 mg/dL in 52%. BM examination was performed in 24.8%. Prevalence of anemia etiologies versus UAE are summarized in Table 1. UAE predominated at 43.7%, followed by IDA at 25%. BM established a hematologic malignancy in 13 (7.5%), including six cases of MDS (4%) and two cases of AML (0.5%). Hematologic parameters in UAE showed the following mean values: Hb of 10.8 g/dL; MCV of 89.9 fL; RDW of 14.6 (normal <15%); and suppressed absolute reticulocyte count at 45.0 K/uL. Only 4/76 (5.3%) of UAE received RBCs within the prior 3 months. Two of these had previously had bleeding and at evaluation had a stable low Hb without an etiology. Thus, in the entire cohort, only 2/29 (6.9%) received RBCs without an explanation. The proportion of AA and whites diagnosed with either UAE or IDA did not differ (p=0.835). Specifically, 23/46 (50%) whites had UAE compared to 48/117 (41.0%) of AA where as 12/26 (26.1%) of whites had IDA and 28/117 (23.9%) of AA had IDA. Figure 1 depicts EPO levels for UAE, IDA, and MDS/AML. Serum EPO levels showed no significant correlation with Hb for UAE (r = - 0.15, p=0.019) but showed a significant inverse correlation with Hb among IDA pts (r = -0.63, p<0.0001). The suppressed EPO in UAE compared to IDA was not explained by renal dysfunction as mean eGFR was 64.2 for UAE versus 60.0 in IDA (p=0.30).
| Diagnosis . | Number (%) . |
|---|---|
| Unexplained | 76 (43.7) |
| Iron Deficiency | 44 (25.3) |
| Inflammation | 17 (9.8) |
| Hematologic Malignancy | 13 (7.5) |
| MDS | 6 (4.0) |
| AML | 2 (0.5) |
| Plasma cell dyscrasia | 3 (1.7) |
| Lymphoproliferative disorder | 2 (1.1) |
| Thalassemia Trait | 8 (4.6) |
| Kidney Disease (i.e., eGFR <30 mL/min/1.73 m2) | 6 (3.5) |
| Hemolytic anemia | 4 (2.3) |
| Alcohol | 3 (1.7) |
| B12 Deficiency | 1 (0.6) |
| Thyroid Dysfunction | 1 (0.6) |
| Medication | 1 (0.6) |
| Folate Deficiency | 0 (0) |
| Diagnosis . | Number (%) . |
|---|---|
| Unexplained | 76 (43.7) |
| Iron Deficiency | 44 (25.3) |
| Inflammation | 17 (9.8) |
| Hematologic Malignancy | 13 (7.5) |
| MDS | 6 (4.0) |
| AML | 2 (0.5) |
| Plasma cell dyscrasia | 3 (1.7) |
| Lymphoproliferative disorder | 2 (1.1) |
| Thalassemia Trait | 8 (4.6) |
| Kidney Disease (i.e., eGFR <30 mL/min/1.73 m2) | 6 (3.5) |
| Hemolytic anemia | 4 (2.3) |
| Alcohol | 3 (1.7) |
| B12 Deficiency | 1 (0.6) |
| Thyroid Dysfunction | 1 (0.6) |
| Medication | 1 (0.6) |
| Folate Deficiency | 0 (0) |
Categories are mutually exclusive.
The data confirm UAE is a hypoproliferative normocytic anemia with suppressed EPO levels that rarely requires RBC transfusions. An intensive hematologic evaluation reveals a wide number of etiologies for anemia among older adults, including 7.5% with hematologic malignancies. Nevertheless, UAE predominates as the most common anemia category in the elderly in both whites and AA's.
Anemia Etiology Among Older Adults
No relevant conflicts of interest to declare.
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal