Abstract
Abstract 3180
Pulmonary embolism (PE) is a continuous risk up to 3 months after surgery. Management of anticoagulation can be challenging in those diagnosed with PE after a major surgical procedure. The aim of this study is to evaluate the outcomes and characteristics of patients diagnosed with PE after a major surgery.
A retrospective cohort of consecutive patients with suspected acute PE that underwent computed tomographic pulmonary angiography (CTPA) or lung ventilation/perfusion scans between 1 January 2007 and 31 December 2008 was constructed by two independent investigators by reviewing each patient's diagnostic images. Patients were included in the study if they had a major surgical procedure (admitted to the hospital for more than 24 hours) and developed PE within 12 weeks of the operation. Patients' follow-up for the first 3 months was recorded. Outcomes included major bleeding, as defined by the ISTH guidelines; recurrent venous thromboembolism (VTE), including PE or deep vein thrombosis (DVT); and mortality. The number of days between treatment initiation and major hemorrhage, recurrent VTE, or death, was recorded.
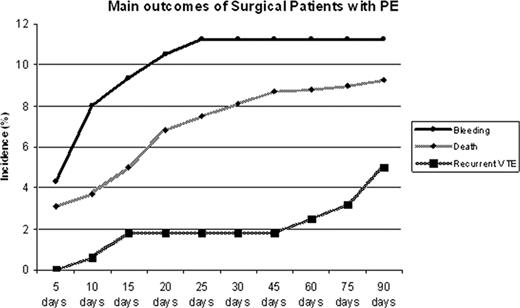
Out of the 842 patients diagnosed with PE at the Ottawa Hospital within the timeframe of the study, 160 (19%) were diagnosed during the post-operative period and were eligible for this study. The mean age (SD) in years was 63 (±15.5), 53% were males, 37% had a cancer related surgery, 37% had orthopedic procedures, and 31% had emergency procedures. The mean time (SD) from surgery to PE diagnosis was 13 (±11) days. All patients were followed-up until the end of their treatment; six patients were transferred to end of life care. Initial treatment was low molecular-weight heparin (LMWH) in 124 (78%) patients, unfractionated heparin (UFH) was given intravenously in 27 (17%) patients, and 5 (3%) requiered an inferior vena cava (IVC) filter to be inserted as the initial treatment. During the 90 days of follow up, there were 17 major bleeding events (12%), 6 recurrent VTEs (4%), and 15 deaths (9%). Of the 17 bleeding events, 13 of them (76%) occurred within the first two weeks of initiation of therapy. No bleeding events occurred after the first month. Two patients died (11.7%) from bleeding, one intracranial and one gastrointestinal (GI). Bleeding was from the GI tract in 47% of cases. Of the 5 patients with IVC filters, 3 developed recurrent DVT in the first two weeks after IVC insertion. The other 3 recurrent VTEs occurred on patients receiving anticoagulation. All cause mortality was 8.7% at 3 months. Within the first 14 days, 8 patients died (5%): 3 patients from PE. Outcomes did not vary by type of surgery, initial treatment or by presence of malignancy.
Major bleeding is a common and deadly complication in patients diagnosed with PE after a major surgical procedure. The reported rates of bleeding in this population have varied widely in the literature (between 2 to 9%), according to the type of surgery or population. Our results suggest that alternative triaging and treatment strategies may be indicated in these patients.
Main outcomes of surgical patients developing pulmonary embolism within 3 months of surgery. Main outcomes were major bleeding, death, and recurrent venous thromboembolism within 90 days of post-operative PE diagnosis. Incidence of outcomes are represented as a percent.
Main outcomes of surgical patients developing pulmonary embolism within 3 months of surgery. Main outcomes were major bleeding, death, and recurrent venous thromboembolism within 90 days of post-operative PE diagnosis. Incidence of outcomes are represented as a percent.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal