Abstract
Abstract 2881
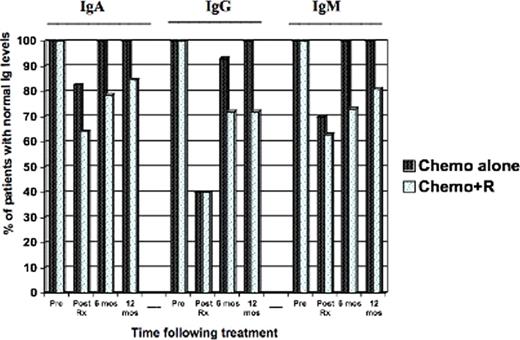
While the delayed effects of rituximab on immune reconstitution are poorly understood, hypogammaglobulinemia has been reported in relapsed patients treated with rituximab. With the widespread use of rituximab, the risk of hypogammaglobulinemia and increased susceptibility to serious infections needs to be formally evaluated. Furthermore, the long-term benefit of rituximab, such as during maintenance schedules, needs to be weighed against potential immunodeficiency. We set out to investigate if rituximab was associated with prolonged hypogammaglobulinemia in previously untreated patients with aggressive B-cell lymphoma (diffuse large B-cell lymphoma (DLBCL) and Burkitt lymphoma (BL)) receiving immunochemotherapy compared to chemotherapy alone. All patients received DA-EPOCH [dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin] with or without rituximab 375 mg/m2 per cycle for 6–8 cycles. We measured sequential IgA, IgG and IgM immunoglobulin levels pre-treatment, at the end of treatment and at 6 and 12 months after treatment. We included samples from 99 patients: 81 received DA-EPOCH-R and 18 received DA-EPOCH alone. Characteristics were similar among patients who received DA-EPOCH-R or chemotherapy alone: male sex 49% v 44%; median age 39 years (18 – 85) v 46 years (20-64); histology DLBCL in 85% v 78% and BL in 15% v 22%, respectively. All patients were HIV negative and in remission at the time of the analysis. We first looked at the effect of chemotherapy alone (DA-EPOCH) on immunoglobulin levels and demonstrated that it induced significant reductions in immunoglobulins by the end of therapy: signed rank p-values were 1.5×10-5 for IgA, 1.5×10-5 for IgG and 1×10-4 for IgM. However, by 12 months after treatment, these changes from baseline had resolved and were no longer significant. Patients who received immunochemotherapy had very significant decrements in all immunoglobulins at the end of therapy – p=5.23×10-13 for IgA, 1.34×10-13 for IgG and 1.36×10-13 for IgM – and these remained significantly lower than baseline at 12 months following therapy – p=9.8×10-12 for IgA, 2.4×10-11 for IgG and 4.1×10-9 for IgM. Next, using Wilcox rank p-values, we compared the median immunoglobulin change (+or-) between the 2 groups at different time points. These were not significant at the end of therapy (p=0.17 for IgA, 0.059 for IgG and 0.97 for IgM) but highly significant for IgA (0.024) and IgG (0.0002) at 12 months following treatment, reflecting persistent immunoglobulin decrements in patients who received rituximab. Next, in patients who had normal immunoglobulin levels at baseline, we compared the proportion in both groups who maintained normal levels at several time points following therapy and this is represented in the chart below. This study, for the first time, demonstrates that in previously untreated patients with aggressive B-cell lymphoma, chemotherapy alone is associated with significant immunoglobulin decrements but these are short-lived and all patients recover normal immunoglobulins by 12 months after therapy. In contrast, immunochemotherapy with rituximab is associated with more severe decrements and prolonged immunoglobulin deficiency that lead to clinically significant reductions, even at 12 months following completion of therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal