Abstract
Abstract 2390
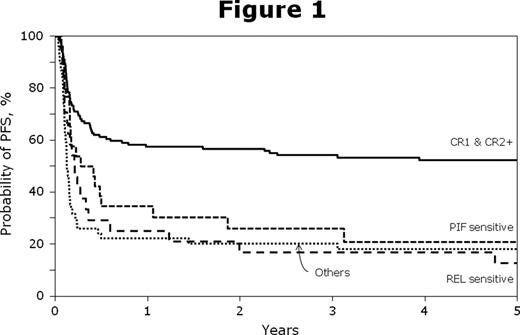
Burkitt lymphoma (BL) is an aggressive B cell lymphoma primarily affecting children and young adults and is characterized by the highest doubling time of any tumor. Cyclical intensive chemotherapy and rituximab confer high complete remission (CR) rates and 80% long term disease free survival in chemotherapy sensitive disease. The role of autologous (autoHCT) or allogeneic (alloHCT) transplant is not well described in BL. We report the outcomes of 241 recipients of HCT for BL between 1985 and 2007 reported to the CIBMTR. Five patients (pts) received syngeneic twin grafts in addition to autoHCT in 113 pts, HLA identical sibling alloHCT (SIB) in 80 pts and mismatched related or unrelated donor (UNR/MM) alloHCT in 48 pts. Baseline patient and disease related risk factors varied significantly between cohorts (table1). The autoHCT cohort had a higher proportion of pts with chemotherapy sensitive disease (86%), peripheral blood grafts (73%) and HCT in first CR (42%). In the UNR/MM cohort, 25% pts were chemotherapy resistant and only 6% were in CR1. The use of autoHCT has declined in recent years with the majority (81%) performed before 2001. Conditioning regimen for alloHCT was myeloablative in 88% (86% and 92% in SIB and UNR/MM respectively). Treatment related mortality (TRM) was higher in alloHCT recipients (table1). Cumulative incidence of relapse/progression at 5 yrs (95% CI) was 44 (35-53)% for autoHCT, 42(31-53)% for SIB and 48 (34-62)% for UNR/MM. For autoHCT, 5-yr progression free survival (PFS) was 48(39-58)%, 78% for those in first CR versus 27% for disease beyond CR1 (p<0.001). For alloHCT, 5-yr PFS was 50% for those in first CR versus 19% for disease beyond CR1 (p=0.001) (figure 1). 5-yr PFS was 30 (20-41)% for SIB and 22 (12-35)% for UNR/MM. Progressive BL was the commonest cause of death.
While autoHCT and alloHCT are both feasible in patients with BL, the use of autoHCT appears to be declining in recent years concomitant with the advent of modern chemotherapy. AlloHCT was performed in those with considerably higher risk disease. Approximately one fifth of advanced BL pts receiving alloHCT beyond CR1 had long term disease free survival.
| Variable . | AUTO . | SIB . | UNR/MM . |
|---|---|---|---|
| N | 113 | 80 | 48 |
| Karnofsky score ≥90 | 67% | 61% | 50% |
| Median age | 31 (5–76) | 24 (3–55) | 22 (2–54) |
| Median time diagnosis prior to HCT, mo | 7 (2–74) | 6 (1–29) | 9 (1–113) |
| Bone marrow involvement @ diagnosis | 22% | 21% | 27% |
| CR1 disease status prior to HCT | 42% | 34% | 6% |
| Chemosensitive disease prior to HCT | 86% | 77% | 71% |
| TRM @ 1 yr (95% CI) | 5 (2–10) | 26 (17–37) | 28 (16–41) |
| PFS @ 5 yr (95% CI) | 48 (39–58) | 30 (20–41) | 22 (12–35) |
| OS @ 5 yr (95%CI) | 54 (44–63) | 32 (22–43) | 23 (12–36) |
| Variable . | AUTO . | SIB . | UNR/MM . |
|---|---|---|---|
| N | 113 | 80 | 48 |
| Karnofsky score ≥90 | 67% | 61% | 50% |
| Median age | 31 (5–76) | 24 (3–55) | 22 (2–54) |
| Median time diagnosis prior to HCT, mo | 7 (2–74) | 6 (1–29) | 9 (1–113) |
| Bone marrow involvement @ diagnosis | 22% | 21% | 27% |
| CR1 disease status prior to HCT | 42% | 34% | 6% |
| Chemosensitive disease prior to HCT | 86% | 77% | 71% |
| TRM @ 1 yr (95% CI) | 5 (2–10) | 26 (17–37) | 28 (16–41) |
| PFS @ 5 yr (95% CI) | 48 (39–58) | 30 (20–41) | 22 (12–35) |
| OS @ 5 yr (95%CI) | 54 (44–63) | 32 (22–43) | 23 (12–36) |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal