Abstract
Abstract 2365
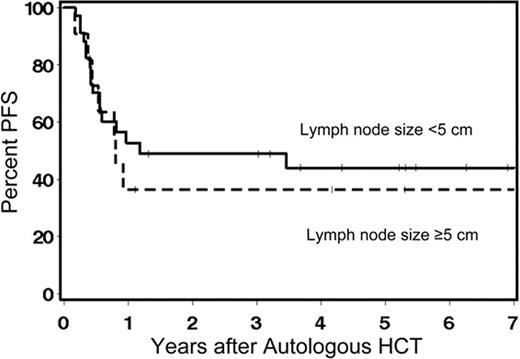
Large lymph node size or chemo-refractoriness limited the success of nonmyeloablative allogeneic HCT in eradicating CLL or lymphoma. We explored an approach of combining the cyto-reductive effect of high dose chemo/radiation therapy and autologous HCT with the graft-versus-tumor effect of nonmyeloablative allogeneic HCT for pts with rapidly progressive/refractory CLL or lymphoma. Between 4/2000 and 3/2010, 45 pts with advanced indolent (16%) or aggressive (54%) non-Hodgkin lymphoma (NHL), Hodgkin lymphoma (HL, 18%), or CLL (11%) ineligible for myeloablative allogeneic HCT due to age and/or comorbidities were treated with the sequential approach. Autologous HCT alone was thought to be insufficient for disease control. Pts received high-dose therapy and autologous HCT followed [at a median of 65 (range 39–128) days] by nonmyeloablative conditioning and related (n=28) or unrelated donors (n=17) allogeneic HCT. Median pt age was 49 (range 20–71) years and number of prior regimens was 4 (range 1–12). Thirty-four percent of pts had disease responsive to the last chemotherapy before autografting [30% partial (PR) and 4% complete remission (CR)] while 44% and 22% had refractory and progressive disease, respectively. Most pts had aggressive disease (72%). Conditioning for autografts consisted of BEAM (49%) or Cyclophosphamide/12 Gy TBI±VP16 (51%). After auto-grafting, 58% of pts had CR/PR (29%/29%), 36% had responses <PR, 3% had relapse, and 3% had refractory disease. Conditioning for allografts consisted of 2 Gy TBI alone (53%) or combined with FLU (47%), 90 mg/m2. Pts received G-CSF mobilized allogeneic peripheral blood mononuclear cells. All 45 pts had sustained donor engraftment. Incidences of grades II, III, and IV acute and of chronic GVHD were 46%, 16%, 0%, and 52% respectively. With median follow up of 51 (range 5–116) months, the overall response rate was 60% (46% CR). Eighteen pts died, 12 from progression/relapse, 3 from pulmonary complications, 1 from GVHD, 1 from sepsis, and 1 from multi-focal leuko-encephalopathy. Estimated 5-year rates of non-relapse mortality, relapse, overall, and progression-free survivals from the time of autografting were 15%, 44%, 55%, and 42% respectively. Pts with CLL or indolent NHL had rates of relapse and PFS of 11% and 68% compared to 47% and 37% for those with aggressive NHL and 69% and 31% for those with HL, respectively. No statistical significant differences in outcomes were detected for lymph node size (Figure), disease status at allografting, donor type, conditioning regimens for autografts or allografts, HCT-comorbidity index scores, or time between autologous and allogeneic grafting (Table). Sequential Auto-Allo HCT resulted in relatively low NRM with median survival not yet reached among pts with rapidly progressive lymphoma/CLL. This sequential transplant approach overcame the previously reported high relapse risk of bulky lymphadenopathy.
Univariate outcomes in 45 patients with CLL/lymphoma receiving sequential autologous and allogeneic nonmyeloablative HCT
| Factor . | Group . | 5 year outcomes (%) . | |||
|---|---|---|---|---|---|
| PFS . | Rel . | NRM . | OS . | ||
| Histology | CLL or Indolent NHL | 68 | 11 | ||
| Aggressive NHL | 37 | 47 | |||
| HL | 31 | 69 | |||
| HR | 3.17 | 6.79 | |||
| 2.49 | 7.20 | ||||
| p-value | 0.12 | 0.04 | |||
| Lymph node size | <5 cm | 44 | 40 | ||
| ≥5 cm | 36 | 55 | |||
| HR | 1.19 | 1.45 | |||
| p-value | 0.70 | 0.47 | |||
| Disease status after autografts | Chemo-responsive | 40 | 38 | ||
| Chemo-refractory | 46 | 43 | |||
| Untested relapse | 36 | 52 | |||
| HR | 1.07 | 1.31 | |||
| 1.38 | 1.75 | ||||
| p-value | 0.83 | 0.68 | |||
| Autografts conditioning regimen | Non TBI-based | 32 | 53 | 15 | |
| TBI-based | 51 | 34 | 14 | ||
| HR | 0.59 | 0.54 | 0.77 | ||
| p-value | 0.20 | 0.20 | 0.75 | ||
| Allografts conditioning regimen | TBI | 47 | 45 | 8 | |
| Flu/TBI | 32 | 44 | 24 | ||
| HR | 1.61 | 1.24 | 3.63 | ||
| p-value | 0.25 | 0.66 | 0.12 | ||
| HCT-CI scores at allografts | 0-2 | 13 | 61 | ||
| 3+ | 15 | 49 | |||
| HR | 1.57 | 1.48 | |||
| p-value | 0.63 | 0.44 | |||
| Interval between autografts and allografts | ≤60 days | 20 | 53 | ||
| >60 days | 11 | 53 | |||
| HR | 0.47 | 0.84 | |||
| p-value | 0.36 | 0.72 | |||
| Donor | Related | 44 | 46 | 11 | 59 |
| Unrelated | 34 | 43 | 23 | 43 | |
| HR | 1.25 | 1.01 | 2.35 | 1.51 | |
| p-value | 0.60 | 0.99 | 0.30 | 0.41 | |
| Factor . | Group . | 5 year outcomes (%) . | |||
|---|---|---|---|---|---|
| PFS . | Rel . | NRM . | OS . | ||
| Histology | CLL or Indolent NHL | 68 | 11 | ||
| Aggressive NHL | 37 | 47 | |||
| HL | 31 | 69 | |||
| HR | 3.17 | 6.79 | |||
| 2.49 | 7.20 | ||||
| p-value | 0.12 | 0.04 | |||
| Lymph node size | <5 cm | 44 | 40 | ||
| ≥5 cm | 36 | 55 | |||
| HR | 1.19 | 1.45 | |||
| p-value | 0.70 | 0.47 | |||
| Disease status after autografts | Chemo-responsive | 40 | 38 | ||
| Chemo-refractory | 46 | 43 | |||
| Untested relapse | 36 | 52 | |||
| HR | 1.07 | 1.31 | |||
| 1.38 | 1.75 | ||||
| p-value | 0.83 | 0.68 | |||
| Autografts conditioning regimen | Non TBI-based | 32 | 53 | 15 | |
| TBI-based | 51 | 34 | 14 | ||
| HR | 0.59 | 0.54 | 0.77 | ||
| p-value | 0.20 | 0.20 | 0.75 | ||
| Allografts conditioning regimen | TBI | 47 | 45 | 8 | |
| Flu/TBI | 32 | 44 | 24 | ||
| HR | 1.61 | 1.24 | 3.63 | ||
| p-value | 0.25 | 0.66 | 0.12 | ||
| HCT-CI scores at allografts | 0-2 | 13 | 61 | ||
| 3+ | 15 | 49 | |||
| HR | 1.57 | 1.48 | |||
| p-value | 0.63 | 0.44 | |||
| Interval between autografts and allografts | ≤60 days | 20 | 53 | ||
| >60 days | 11 | 53 | |||
| HR | 0.47 | 0.84 | |||
| p-value | 0.36 | 0.72 | |||
| Donor | Related | 44 | 46 | 11 | 59 |
| Unrelated | 34 | 43 | 23 | 43 | |
| HR | 1.25 | 1.01 | 2.35 | 1.51 | |
| p-value | 0.60 | 0.99 | 0.30 | 0.41 | |
Note: p-values reflect hazard ratios over all follow-up period
5-years progression-free survival of 44% and 36% for CLL/lymphoma pts with lymph node size of <5 vs. ≥5cm after sequential autologous and allogeneic nonmyeloablative HCT.
5-years progression-free survival of 44% and 36% for CLL/lymphoma pts with lymph node size of <5 vs. ≥5cm after sequential autologous and allogeneic nonmyeloablative HCT.
Off Label Use: All discussions about therapeutics used for HCT preparative regimens are off-label.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal