Abstract
Abstract 2360
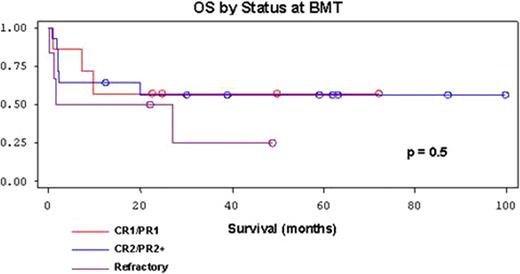
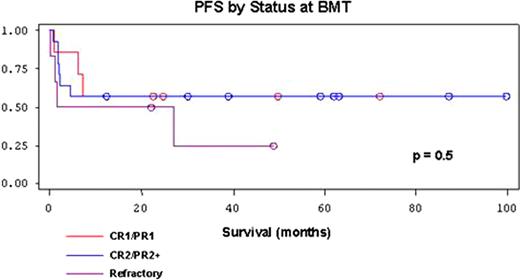
Peripheral T-cell lymphomas (PTCL) represent a rare and heterogeneous group of lymphoproliferative disorders characterized by poor prognosis. For relapsed and refractory disease, treatment options remain limited, and recent data has suggested that patients with PTCL beyond first remission (CR2/PR2+) do not benefit from autologous hematopoietic stem cell transplantation (HSCT) (Chen et al. Biol Blood Marrow Transplant. 2008; 14:741-747). The role of allogeneic HSCT in this patient population is not well defined, although several recently published retrospective analyses have shown promising results. We examined the outcomes of 27 patients with PTCL who underwent allogeneic HSCT for relapsed or primary refractory disease at Washington University between 1997–2008. PTCL subtypes in this cohort included PTCL not otherwise specified (NOS,n=9), anaplastic large cell lymphoma (ALCL,n=9), angioimmunoblastic T-cell lymphoma (AILT,n=5), hepatosplenic gamma-delta T-cell lymphoma (n=2), subcutaneous panniculitis-like T-cell lymphoma (n=1), and extra-nodal NK T-cell lymphoma (n=1). Among the patients with ALCL, 1 patient had anaplastic lymphoma kinase (ALK) negative ALCL; however, ALK status was unavailable for the other 8 patients in this group. Median age was 45 years (range 19–61) and 37% were female. 23 patients underwent myeloablative conditioning regimens with the majority receiving total body irradiation and cytoxan (74%). 4 patients received nonmyeloablative conditioning regimens consisting of fludarabine and anti-thymocyte globulin. 14 patients had HLA-identical related donors, 8 patients had HLA-identical unrelated donors, and the remaining 5 patients had unrelated mismatched donors. In general, patients were heavily pre-treated with an average of 3.3 chemotherapy regimens preceding allogeneic HSCT, and 7 patients (26%) had undergone prior autologous HSCT. 7 patients were transplanted at CR1/PR1, 14 patients at CR2/PR2+, and 6 patients had refractory disease at the time of transplant. Of the patients that were transplanted at CR1/PR1, 6 out of 7 were refractory to their first-line chemotherapy. 1-year, 3-year, and 5-year overall survival (OS) rates were 59%, 50%, and 50%, respectively. Corresponding progression free survival (PFS) rates were 56%, 51%, and 51%, and non-relapse mortality (NRM) rates were 15%, 15%, and 15%. Median OS was 27 months, and median follow-up time was 22 months. Univariate analysis demonstrated similar rates of OS (p=0.5), PFS (p=0.5), and NRM (p=0.8) between the CR1/PR1 and CR2/PR2+ subgroups, and a trend towards lower OS and PFS in patients with refractory disease at transplant. There was no statistical difference in OS (p=0.6), PFS (p=0.6), or NRM (p=0.6) between different PTCL histological subtypes, and no clear trend favoring any particular subtype. We conclude that allogeneic HSCT can provide durable remission and survival for patients with relapsed and refractory PTCL, with acceptable treatment-related mortality. Future prospective trials are needed to further define the role of allogeneic HSCT in this patient population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal