Abstract
Abstract 2324
Infectious as well as non-infectious pulmonary complications are key determinants of non-relapse mortality (NRM) after allogeneic hematopoietic stem cell transplantation (allo-HSCT). Single nucleotide polymorphisms (SNP) in two genes coding for nucleotide-binding oligomerization domain containing 2 (NOD2) and bactericidal/permeability-increasing protein (BPI) have been shown to predict for the occurrence of GvHD and chronic pulmonary complications after allo-HSCT. We aimed at determining the effect of SNPs in these genes on the occurrence of acute lung injury (ALI) after allo-HSCT.
We retrospectively analyzed a cohort of 272 patients undergoing allo-HSCT and their respective related and unrelated donors. ALI was functionally defined as a drop of the oxygenation index (OI = partial pressure of oxygen in arterialized capillary blood/inhaled oxygen concentration) below 300. Genotyping for NOD2 SNP 8, 12 and 13 and BPI SNP A645G was done using Real Time-PCR. The incidence of ALI was assessed by univariate competing events statistics and by a multivariate model according to Fine and Gray.
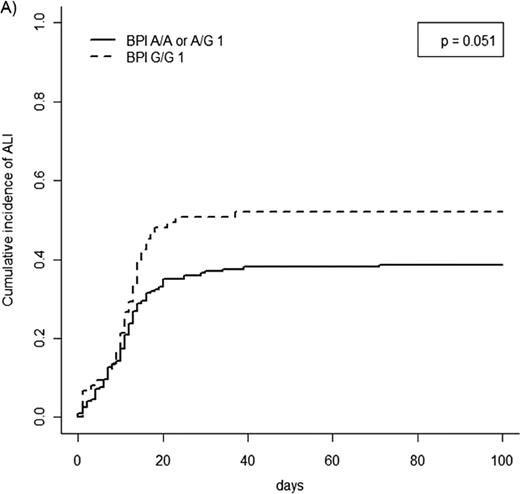
Overall, 115 of 272 (42.3%) patients suffered from ALI at least once during the first 100 days post allo-HSCT. Median time to onset was 11 days. Neither NOD2 polymorphisms in the donor nor in the recipient correlated with the occurrence of ALI. Further, BPI recipient genotype was not associated with an increased incidence of this complication. On the other hand, ALI was more frequent in patients receiving a transplant from a donor homozygous for the G allele of the BPI A645G SNP (Figure 1). This association was confirmed in multivariate analysis (OR 1.46, p = 0.048). Other independent risk factors for the occurrence of ALI were age (as continuous variable, OR 1.03, p = 0.002) and transplantation from an unrelated vs. related donor (OR 1.66, p = 0.018) whereas the use of intensive conditioning was a risk factor of borderline significance (OR 1.59, p = 0.077). In spite of its association with ALI, BPI donor genotype did not correlate with cumulative incidence of NRM at 100 days (G/G: 6.7%, 95% CI: 1.0 – 12.4% vs. A/A or A/G: 10.2%, 95% CI: 6.0 – 14.4%; p = 0.380) or overall survival.
In contrast to other investigators we found no correlation between NOD2 genotype and the occurrence of acute pulmonary complications after allo-HSCT. On the other hand, BPI A645G SNP in the donor was identified as an independent risk factor for ALI in these patients.
Cumulative incidence of ALI according to BPI genotype
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal