Abstract
Abstract 2317
The polyoma virus BK is present in the urothelial tract of the majority of patients undergoing allogeneic hematopoietic stem cell transplantation (HSCT). Urothelial damage by the conditioning regimen triggers early viral replication and subsequent immune mediated damage to the urothelium. Clinical manifestations of BK virus-associated hemorrhagic cystitis (BKHC), with typical onset in the first 100 days after HSCT, range from asymptomatic microscopic hematuria to massive life threatening blood loss and urinary obstruction. There is no standard prophylaxis or treatment for BKHC. The antibacterial fluoroquinolones have been shown in vitro to inhibit BK viral replication by direct inhibition of the BK encoded DNA gyrase. Therefore, we hypothesized that extended prophylaxis with the fluoroquinolone ciprofloxacin might decrease the incidence of severe BKHC after HSCT.
In March 2009 we began prescribing prophylaxis for BKHC with ciprofloxacin 500 mg orally twice daily from day 0 until day 60 after transplantation in all allograft recipients (except patients allergic to ciprofloxacin). Patient and transplant variables, as well as incidence of severe BKHC, were collected retrospectively for all consecutive patients undergoing allogeneic HSCT between June 2006 and July 2010. Severe BKHC was defined as grades 3 or 4 hemorrhagic cystitis with evidence of urinary excretion of BK virus by polymerase chain reaction. We estimated the incidence of severe BKHC and the survival free of severe BKHC for patients receiving (ciprofloxacin group) or not (control group) prophylaxis. Additionally, we performed a multivariate analysis to assess the independent role of ciprofloxacin prophylaxis in preventing episodes of severe BKHC.
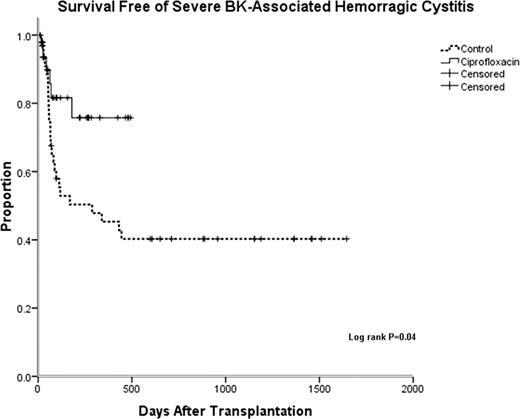
Eighty-one consecutive patients were included in the analysis, of which 33 received ciprofloxacin prophylaxis. Median age of patients was 50 years (range 19–70) and 37% were female. Overall 47% of patients received a myeloablative conditioning regimen and 60% had an alternative (not HLA-matched sibling) donor. Median follow up for patients in the ciprofloxacin and control groups were respectively 180 (range 33–504) and 515 days (range of 29–1645). There was no difference in overall survival between ciprofloxacin and control groups. Episodes of severe BKHC occurred after a median of 60 days (range 27–118) after transplantation and were less frequent in the ciprofloxacin than in the control group (2.9% vs. 22.9%, chi-square test P= 0.01). Survival free of severe BKHC was also significantly superior in the ciprofloxacin group (Log-rank test P=0.04; Figure). In a multivariate Cox-regression analysis including age, gender, intensity of the conditioning regimen, use of mesna during conditioning and alternative donor, only the use of ciprofloxacin prophylaxis was significantly associated with the endpoint survival free of severe BKHC (P=0.01). There were no complications associated with prolonged use of ciprofloxacin, in particular no increase in Clostridium difficile associated diarrhea.
Ciprofloxacin prophylaxis appears safe and effective in reducing the incidence of severe BKHC after allogeneic HSCT. This finding requires confirmation with a prospective randomized trial.
Off Label Use: Ciprofloxacin- prevention of BK associated hemorragic cystitis.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal