Abstract
Abstract 2274
Patients with CML in chronic phase who have failed imatinib therapy are commonly treated with dasatinib or nilotinib, but a significant proportion fail to respond or relapse in which case they are often treated with the other tyrosine kinase inhibitor (TKI) that they had not yet received. We report here the largest series of CML patients in CP treated with a third line TKI after failing both imatinib and another TKI.
We enrolled 26 patients. The median age was 64 years and 54% were male. 20 patients had received dasatinib and 6 nilotinib as second line therapy. All patients were still in first CP at the moment of commencing third line therapy, and none was harboring a T315I mutation. Failure to second line therapy was defined as no CHR at 3 months, no major cytogenetic response (MCyR) at 12 months or loss of a hematological or cytogenetic response. Patients who were unable to continue therapy on account of toxicity were also considered as having failed therapy. The median follow up for the surviving patients after starting third line therapy was 21.5 months (range, 6 – 46.5 months).
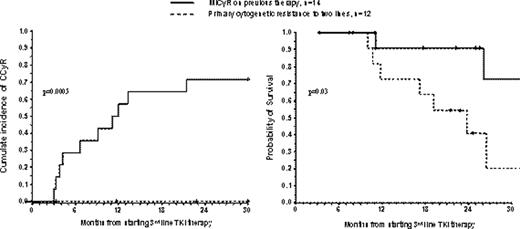
The 2.5 years (30 months) cumulative incidences of MCyR, CCyR and MMR were 48.2%, 32.4%, 21.1% respectively. Multivariate analysis showed that the achievement of at least MiCyR (<95% Ph-positive) on imatinib (RR=5.6, p=0.03) or on second line therapy (RR=11.8, p=0.006) were the only independent predictors for the achievement of CCyR. When combining both variables we found that patients who had achieved MiCyR on one of the two prior therapies had a significantly better OS and higher probability of achieving cytogenetic response on third line therapy, i.e. the 30 month probability of OS and CCyR were 72.7% vs 20.4% (p=0.03) and of 71.4% vs 0% (p=0.0005) respectively (Figure).
During follow up 9 (34.6%) patients died. The probability of OS at 30 months was 46.7%. The achievement of a cytogenetic response on second line and age younger than 64 (possibly reflecting eligibility for transplantation) were the only independent predictors for OS (RR=6.5, p=0.02 and RR=0.13, p= 0.02).
Seventeen patients (65%) were classified as intolerant to previous therapies (imatinib or second line TKI). Intolerant patients had a probability of responding to the third line therapy similar to those of the resistant patients, but when this cohort was subdivided according to the type of intolerance we found that 11 patients who had hematologic toxicity with either therapy had a probability of CCyR at 30 months lower than that of the remaining 15 patients (11.1% vs 47.5 %, p=0.03), while the 8 patients with non-hematologic intolerance to the imatinib or to the second line had a probability of 30-month CCyR greater than that of the remaining 18 patients (87.5% vs 5.6%, p<0.001).
At 3 months 26 patients remained on follow up, of whom 9 patients had achieved at least MiCyR. These 9 patients had better 30-month probabilities of CCyR and OS than the patients who had failed to achieve MiCyR, namely 88.9% vs 13.3% (p<0.0001), and 87.5% vs. 35.0% (p=0.1). When we excluded the only patient who died of non-leukemia related causes while in CCyR, the probabilities of OS was 100% vs 35.0% (p=0.04)
Which patients should be offered third line TKI therapy? Patients who achieved cytogenetic response on first or second line therapy and patients with a history of non-hematologic intolerance to the prior TKI benefited from a third TKI. Patients with primary cytogenetic resistance to two TKIs or with a history of hematologic intolerance should receive an allogeneic stem cell transplant when possible. For patients in this situation who lack a transplant option we would recommend only a short course (3 months) of the third line therapy to identify responders. Non-responders should be offered experimental studies.
Marin: Bristol-Myers Squibb: Consultancy; Novartis: Consultancy, Research Funding.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal