Abstract
Abstract 2266
We conducted a national retrospective analysis on 63 patients (pts) with either myeloid or lymphoid BC CML who underwent a first allogeneic stem cell transplantation as consolidation therapy for BC, since 2000 in France and look at whether 1st and 2nd generation TKIs ±chemotherapy prior to transplant may impact on outcome. There were 46 males and 17 females, and the median age at transplant was 34 (range 3–63) years and the median delay between BC and transplant was 19.6 (2.3-113) months. Thirty six (57%) pts were in chronic phase (CP), 3 (5%) in accelerated and 24 (38%) in BC at CML diagnosis. Twenty three pts received 1 line of treatment, 26 pts 2 lines, and 14 pts 3 or more lines for CML treatment before BC. For BC treatment, 25/63 (39%) pts had chemotherapy without TKI and 29/63 (46%) had TKIs combined or not to chemotherapy (6 chemo+dasatinib, 4 chemo+imatinib, 8 dasatinib alone, 1 dasatinib and imatinib, 9 imatinib, 9 unknown). At transplant 35/63 (55%) were considered in 2nd CP and 28 (45%) still in BC. The majority of the pts had an identical sibling donor (42/63: 66%), 1 mismatched related, 7 matched unrelated, and 13 mismatched unrelated. Fifty-six (89%) pts had a standard conditioning regimen, 7 (11%) pts a RIC regimen and 39 (62%) had a TBI. The stem cell source was bone marrow in 33/63 (52%) pts, PBSC in 24/63 (38%) and cord blood for 6/63 (10%). Fourteen transplants were sex-mismatched (female donor for male recipient). The EBMT-Gratwohl score was low (1+2+3) for 35/63 (55%) pts, intermediate (4) for 14 pts and high (5) for 9 pts, (and 6) for 3 pts and undetermined for 2 pts. The median follow-up since transplant was 25 (range 0.43–109) months. The overall median time for neutrophil recovery (neutrophils > 0.5 109/l) was 20 days. Fourty-one (65%) pts had an aGVHD (29 grade i-II and 12 grade III-IV) with no statistical differences between stem cell sources (p=0.4 for cord vs BM and 0.58 for PBSC vs BM). The cumulative incidence of chronic GVHD (14 extensive, 10 limited) was 43% at latest follow-up, more frequent in RIC transplant. The cumulative incidence of CML relapse was 38% at 2 yrs and multivariate analysis demonstrated the significant impact on relapse of the status at transplant in favour of disease control prior to transplant [HR 2.22 (1-4.93, p=0.05] and unexpectedly, no impact of BC treatment with or without TKIs prior to transplant and of other variables. The median overall survival (OS) was 22 months (see Figure 1).
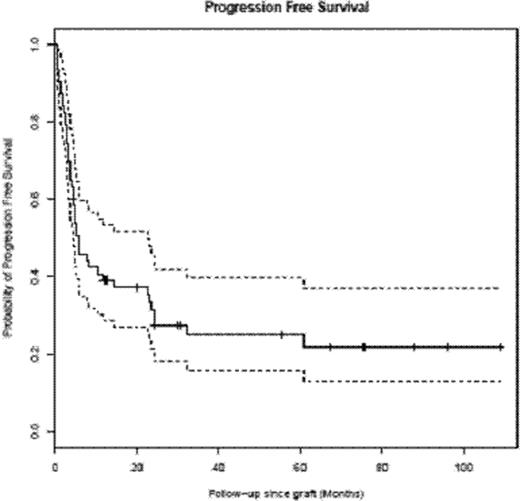
The TRM was 33% at latest follow-up, and it was significantly negatively influenced by the EBMT score (p=0.0077 for scores ≥ 4), BC status at diagnosis (p=0.04). The OS was not improved when using standard conditioning regimens (p=ns), but was improved by disease status at transplant (2nd CP better than persistent BC, p=0.01) and transplant with cord blood and BM stem cell sources over PBSC (p=0.011). Multivariate analysis on OS detected as significant adverse prognosis factors EBMT score ≥5 (HR=4.63 EBMT 5, and 4.77 EBMT 6). The types of treatment of BC CML had no significant impact (with or without stratification on chemotherapy). The median progression-free survival (PFS) was 5.8 months (see Figure 2).
The PFS was not significantly improved by standard conditioning regimens but again was improved by disease control prior to transplant (2nd CP better than persistent BC, p=0.001) and with cord blood and BM stem cell sources over PBSC (p=0.057). Multivariate analysis on PFS detected as significant adverse prognosis factors EBMT score ≥5 (HR=5.82 EBMT 5, and 3.82 EBMT 6), but again, the types of treatment of BC CML prior to transplant had no significant impact.
In conclusion, this analysis suggests that OS and PFS rates are significantly improved when compared to figures from the pre-TKI era. The use of 1st or 2nd generation TKIs alone or combined to chemotherapy does not seem to influence transplant results. CML status and the EBMT score are the major factors that can significantly influence transplant outcome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal