Abstract
Abstract 2166
An established factor for predicting the mortality of patients admitted to an ICU is the Severe Acute Physiology Score (SAPS) II. However, for patients with acute myeloid leukemia (AML) it is uncertain whether factors beyond SAPS II do influence the ICU outcome. Therefore we examined additional factors including age and factors related to AML biology and its treatment in the so far largest cohort of patients with AML worldwide regarding their ICU outcome.
Retrospective analysis of 256 patients with 366 admissions to medical ICU between 2004 and 2009 in 3 large German hematologic centers. Patient age and gender, reason for ICU admission, duration of intensive care, SAPSII, need for invasive mechanical ventilation (IMV), renal replacement therapy and/or vasopressors, laboratory values at ICU admission for creatinine, bilirubin and C-reactive protein, AML karyotype, presence of FLT3-ITD and/or NPM1-mutation, FAB classification, last AML treatment, AML status and allogeneic transplant status were evaluated as potential risk factors. Correlations were analyzed using the Mann-Whitney U test. Univariate analysis was performed using the log rank test for the time until death on ICU occurred. Significant risk factors were studied in multivariate analysis (Cox regression).
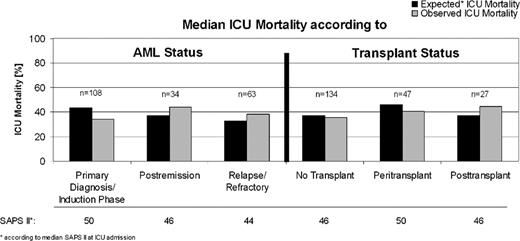
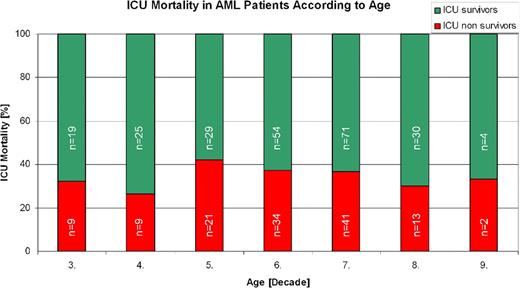
At the time of analysis (08/2010) the median age of patients was 55.3 (range 19.7–84.9) years, and 47.5% were female. 46% of ICU admissions were due to infectious complications. A respiratory problem was present in 60% of the ICU transfers. IMV, vasopressors and renal replacement therapy were necessary in 51.3%, 42.6% and 22.7%, respectively, of the ICU courses. ICU survival was 64.8%. AML status was primary diagnosis/induction phase in 53.3%, postremission phase in 15.8% and relapse/refractory in 27.6% of ICU courses. 66.4% of admissions to ICU had conservative treatment (no transplant), 15.8% underwent allogeneic hematopoietic stem cell transplantation (allo SCT) in the same hospital stay (peritransplant status) and 14.5% had had allo SCT in a former hospital stay (posttransplant status). AML karyotype was favourable in 7.1%, intermediate in 47.8% and unfavourable in 20.2%. SAPS II was available in 208 ICU transfers. Duration of intensive care was 8.1 (mean)/3.0 (median) days with a range from 0.5–76 days. In univariate analysis risk factors predicting diminished ICU survival were high SAPS II (p=0.008), sepsis as reason for ICU admission (p=0.007), need for IMV (p<0.001), use of vasopressors (p<0.001), renal replacement therapy (p=0.002), intermediate or unfavourable AML karyotype (p=0.027), FAB classification other than AML M3 (p=0.012), postremission or relapse/refractory status of AML (p=0.029) and posttransplant status of AML (p=0.002). ICU mortality was lower in primary diagnosis/induction phase and higher in posttransplant phase of AML than predicted by the median SAPS II of these cohorts. In multivariate analysis the only significant predictor of inferior ICU survival was the extent of vasopressor treatment (hazard ratio (hr) 1.83, 95% CI 1.09–3.08; p=0.022), whereas high SAPS II was of borderline significance (hr 1.02, 95% CI 1.00– 1.03; p=0.064).
In contrast to the broad majority of ICU patients, SAPS II is not an optimal predictor of ICU survival in patients with AML. Disease status was of high relevance with an AML status of primary diagnosis/induction phase indicating a better and posttransplant (but not peritransplant) status a worse ICU survival than predicted by SAPS II. The strongest predictor for ICU mortality was the extent of vasopressor use. In contrast age up to the 8th decade had no impact on ICU survival. These results may help to better define ICU admission and treatment policies for patients with AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal