Abstract
Abstract 1782
Chemo immunotherapy (R-CHOP) has improved outcomes of both GC (germinal center) and ABC (activated B-cell) subtypes of DLBCL. However outcomes in DLBCL patients treated with R-CHOP with ABC subtype (vs. GC) and/or with poor-risk features (High IPI, high Ki-67) remain inferior. These patients might benefit from more dose-intensive or high-dose therapy approaches. In our practice at The John Theurer Cancer Center, we have employed a risk-adaptive strategy with R-HCVAD to treat patients with DLBCL with aggressive features.
Utilizing Kaplan Meier (KM) survival and Cox regression analyses, we conducted a retrospective cohort study to describe the outcome of patients treated with R-HCVAD in the 1st-line setting with the following high-risk features: high Ki-67 (MIB-1), high IPI, multiple extra-nodal (EN) sites, bulky disease or immunohistochemistry (IHC) staining patterns (GC vs. non GC by Hans’ model). The primary study endpoints were PFS and OS. The proportional hazards assumption was met for this analysis.
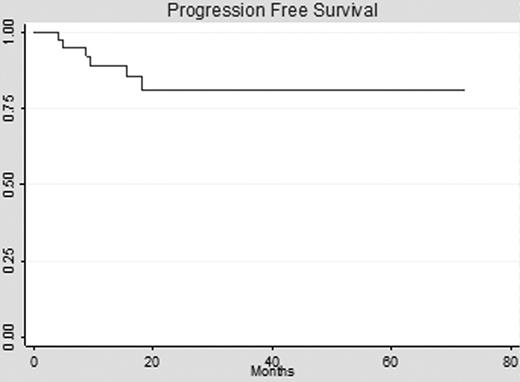
45 patients (median age 57, range 34–71 yrs) with newly diagnosed DLBCL treated with R-HCVAD (median 6 cycles, range 1–8) were available for this analysis, representing 1010 total months of follow up at-risk. Baseline characteristics included: stage III-IV (90%), IPI ≥ 3 (52%), median Ki-67 (80%, range 10–100%), median EN sites (2), non-GC subtype (34%), bone marrow (BM) involvement (38%), EBER positive (14%), HIV negative (100%). With 17 months (range 9–64 months) median follow up, median OS and PFS (graph) are not yet reached. 2-yr PFS and OS were 80% (95% CI 61–91%) and 78% (95% CI 61–88%) respectively. In Cox regression analysis, survival outcomes were not adversely affected by: patient age > 60 (HR .8, p=.18), LDH > ULN (HR 2.3, p=.3), non-GC IHC pattern (HR .5, p=.5), BM involvement (HR 1.9, p=.4), Ki-67 ≥ 80% (HR 1.7, p=.6) or EN sites ≥ 2 (HR 4.7, p=.15).
This analysis represents the largest reported cohort of DLBCL patients treated with R-HCVAD. These data suggest that R-HCVAD can overcome traditional poor-risk features such as high IPI, high Ki-67 and non-GC IHC pattern. Future work will focus on identifying molecular markers for failure in DLBCL patients treated with dose-intensive regimens. A randomized trial comparing R-HCVAD to R-CHOP in selected high-risk patients is warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal