Abstract
Abstract 1764
Cardiovascular System disorders are among the leading causes of mortality in general population ranging from 10% in Sub Saharan Africa, 38 % in Western Europe and US to even 58% in Eastern Europe and Central Asia. CHOP and it's modifications, with or without Rituximab is the most frequently used chemotherapy regimen for lymphoma patients. Antharcyclin related cardiotoxicity is a well described, dose dependent adverse effect, increasing in frequency with time after therapy, described in 3–5% of patients at 5 years to even 15% of patients at 10 or more years after diagnosis. It was postulated, that higher incidence of cardiovascular mortality, may increase the frequency of anthracyclin cardiotoxicity in Central Europe.
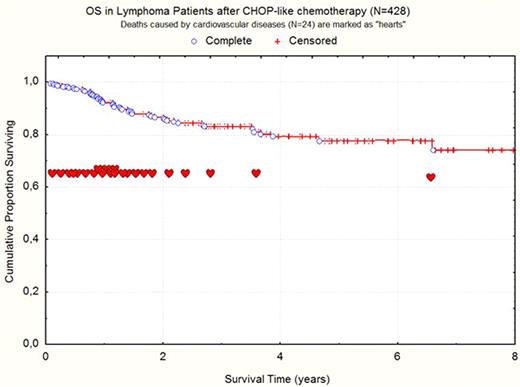
A retrospective analysis was performed to investigate the frequency of cardiovascular complications after CHOP-like chemotherapy in 428 lymphoma patients treated in 5 oncohematological centers. The median observation time was 3 years (range 0.5–8), therefore it covered acute and early chronic progressive cardiotoxicity. Patients characteristics: average age 55 years (range 18–90), male to female ratio 221/207, clinical stage III/IV – 347 cases (81.5%), general symptoms – 302 cases (71%), large tumor burden defined as it's diameter of 10 cm or more – 41 cases (8.5%), IPI 3–5 in 174 cases (40%). There were 320 patients with DLBCL, 45 – MCL, 32 – FL, 24 – PTCL and 7 – MZL. Initial assessment was based on medical histories including echocardiography in 166 cases (38%). All patients were contacted at the time of analysis, and questioned in detail about symptoms and signs of left ventricular failure (LVF).
At a time of diagnosis risk factors for cardiovascular disorders were identified: arterial hypertension (29%), hypercholesterolaemia (13%), diabetes mellitus (8.2%), truncal obesity (17%) and smoking (18.5%). Minority of patients had a previous history of LVF (n=10, 2.3%) and/or myocardial infarction (n=6, 1.4%). The average dose of anthracyclins was 336,5 mg/m2 (range 50 – 680): 391 (91.9%) patients received Doxorubicin, 17 (3.9%) – Nonpegylated Liposomal Doxorubicin, 13 (3,1%) – Farmorubicin and 5 (1.1%) Dauborubicin. Acute cardiotoxicity was reported in 21 cases (4,9%) and resulted in dose reduction, postponing chemotherapy or it's premature termianation. The overall response rate was reasonable, with 297 (69.5%) CR, 83 (19.5%) PR, 10 (2.2%) SD and 38 (8.8%) progressions. At the time of analysis 100 patients (23.4%) relapsed and 63 (14.7%) died: 29 due to disease progression, 24 due to cardiovascular disease, 7 due to infectious complications and 3 due to unknown causes. The average Left Vetricular Ejection Fraction (LVEF), assessed by echochardiography in 166 patients decreased from 63% (range 42–85%) at diagnosis to 56,8% (range 20–72%) at the end of treatment (p<0.001). It corresponded to clinical picture: 51 patients (11.7%) required cardiological treatment after chemotherapy, including 15 cases (3.5%) with myocardial infarction, and further 37 (8.6%) with ischaemic heart pain. Even more revealed signs and symptoms of LVF on direct questioning: exertional dyspnea – 67 (15.7%), pretibial oedema – 72 (16.8%), Nycturia – 48 (11.2%).
Our retrospective analysis revealed an important role of anthracyclin cardiotoxicity in lymphoma patients from Poland. At relatively short average time of observation (3 years, range 0.5–8), cardiovascular disorders were the second most common cause of death (24/63 – 38% of deaths, 24/428 – 5.6% of all cases). Further 51 patients (11.7%) required cardiological treatment for at least one life threatening event (myocardial infarction or ischaemic heart pain).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal