Abstract
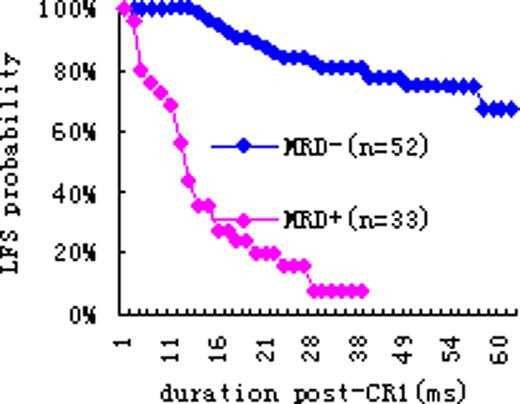
Minimal residual disease (MRD) is the most important factor to predict the prognosis after chemotherapy in the patients with acute leukemia(AL). Among the techniques for MRD detection, flowcytometry (FCM) is both sensitive and feasible tool, which can be used in almost all patients no matter with or without cytogenetic or molecular marker. It has been widely recognized that the MRD by FCM can predict the prognosis of the patients with ALL after several cycles of chemotherapy, but there are few reports on the value of MRD by FCM in AML. To investigate the clinical prognostic value of monitoring MRD regularly with FCM, the correlation of MRD and leukemia-free survival (LFS) in patients with AL without initial high risk factors was studied. From April 2005 to July 2009, 119 newly diagnosed patients (AML 85, ALL 34) and 39 treated cases (AML 19, ALL 20) were included. Those treated patients had attained the first complete remission (CR1) for more than 1 year after chemotherapy in other hospital and then were transferred to our hospital and detected MRD by FCM regularly since then. MRD in bone marrow (BM) was detected every 1 to 3 months in the first year after CR1, and every 2 to 6 months thereafter until hematological or extramedullary relapse or by July 2010. The special antibody combinations were employed for each patient according to aberrant expression of leukemia cells detected by the primary immune phenotype, or antigen drift in the follow-up. MRD was analyzed by the same doctor and assessed according to some abnormal characteristics, including antigen over-expression, antigen low-expression or even loss, co-expression of different lineages or different stage antigens on a single cell, and abnormal patterns in light scatters. MRD+ was defined as the aberrant cells more than 0.01% in BM at the twelfth month for AML and the fifth month for ALL. Among 85 newly diagnosed AML, 33 cases were MRD+ with the median ages 29(4-73)years old, 52 cases were MRD- with the median ages 35(9-68)years old. A total of 2/33 patients in MRD+ group and 40/52 patients in MRD- group remained in LFS. The probability of LFS at 12 months and 24 months was 56% and 16% in MRD+ group, 100% and 84% in MRD- group, respectively (see Figure 1), the difference between MRD+ and MRD- groups was significant statistically (p<0.001). Among 34 newly diagnosed ALL, 13 cases were MRD+ with the median ages 20(12-45)years old, 21 cases were MRD- with the median ages 17(6-35)years old . A total of 1/13 patients in MRD+ and 19/21 patients in MRD- remained in LFS. The probability of LFS at 12 months and 24 months was 46% and 38% in MRD+ group, 95% and 95% in MRD- group(see Figure 2), the difference between MRD+ and MRD- groups was significant statistically (p<0.001). Similar pattern was seen in treated patients. Among 19 treated AML, 0/6 in MRD+ group and 11/13 in MRD- group remained in LFS. Among 20 treated B-ALL, 0/5 in MRD+ group and 14/15 in MRD- group remained LFS. In conclusion, our data indicate that MRD monitored by FCM in both AML and B-ALL correlates to LFS very well. It is important to monitor MRD regularly with FCM in the patients with AL after remission in order to earlier identify high-risk patients for relapse who need intensified treatment, such as allogeneic hematopoietic stem cell transplantation.
LFS probability of AML ±MRD Figure 2: LFS probability of B-ALL ±MRD
LFS probability of AML ±MRD Figure 2: LFS probability of B-ALL ±MRD
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal