Abstract
Abstract 1528
While black patients (pts) have a lower relative incidence of Diffuse Large B cell lymphoma (DLBCL),previous studies have shown that they tend to present at a younger age, with more advanced stage disease and have inferior 2 year and 5 year relative survival rates (ASH 2007 4430a; ASH 2009 898a). These studies have been limited by small numbers of black pts and by being single institution analyses. We performed a combined retrospective analysis of DLBCL pts treated at Emory & University of Alabama at Birmingham (UAB) to examine demographic, clinical, International Prognostic Index (IPI) score, socioeconomic, and treatment variables to determine their impact on survival in black (B) and white (W) pts.
Clinical, pathology, and pharmacy records were reviewed and 862 pts were identified with DLBCL who were evaluated or received treatment at Emory and UAB from 1981–2010. Baseline demographic data, components of the IPI [age, stage, performance status (PS), LDH, number of extranodal sites (ES)], family history of lymphoma, insurance & employment status, as well as treatment and survival data were extracted. Pts with incomplete treatment and outcomes data or unknown race were excluded (n=87) as were n=157 who received treatments other than CHOP or R-CHOP. The primary outcome was overall survival (OS). Differences in baseline features and treatment category were analyzed using Chi-squared statistical analysis. Univariate & multivariate logistic regression analyses were performed for the entire population and cohorts matched by IPI, age, year of diagnosis and socioeconomic factors, to determine predictors of 2-year and 5-year survival.
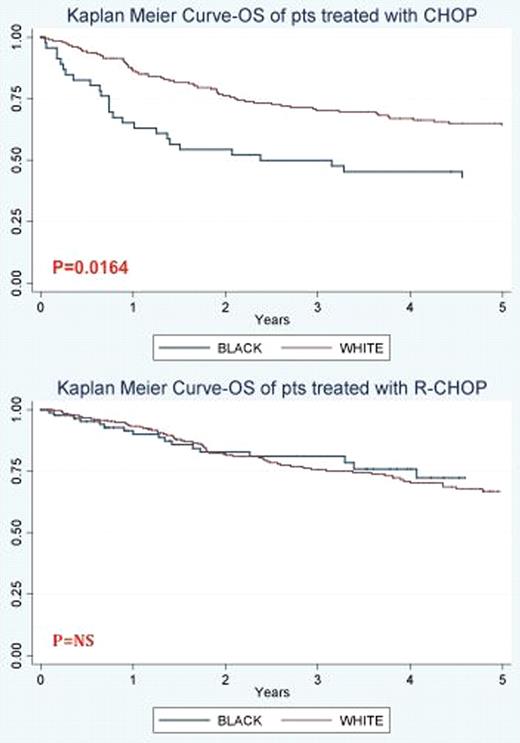
A total of 618 pts with DLBCL (n=484 W, n=134 B) who received either CHOP (n=249) or R-CHOP (n=369) were included in the present analysis. Univariate analyses demonstrated that age >60 yrs, PS 32, ES32, presence of B symptoms, high LDH, and IPI score 32 but not race were each significantly associated with a poorer survival. In multivariate Cox analysis age >60 (Hazard Ratio (HR) 1.5, 95%CI 1.2–2.9), PS 32 (HR 2.6, 95%CI 2.0–3.5), and male sex (HR 1.2, 95%CI 1.0–1.5) (p=0.047) predicted significantly worse survival. Treatment with R-CHOP was associated with significantly better survival (HR 0.6, 95%CI 0.4–0.9). In multivariate models of pts treated with CHOP, white race was associated with significantly better survival (HR 0.6, 95%CI 0.4–0.9) (see Figure) while IPI scores 3–5 (HR 3.1, 95%CI 1.9–4.9) and male sex (HR 1.5, 95%CI 1.0–2.1) were associated with worse survival. However among pts treated with R-CHOP, IPI scores 3–5 (HR 3.2, 95%CI 1.8–5.7) and Medicaid insurance (HR 2.8, 95%CI 1.4–5.5) but not race or gender was associated with worse survival. In multivariate models of pts treated with CHOP, white race was associated with better survival (HR 0.6, 95% CI 0.4–0.9) while IPI scores 3–5 (HR3.1, 95% CI 1.9–4.9) and male sex (HR1.5, 95%CI 1.0–2.1) were associated with worse survival. Univariate & multivariate analysis of 2-yr OS and 5-yr OS also demonstrated that IPI scores 3–5, and all IPI components individually were associated with significantly worse survival. In both univariate and multivariate analysis, treatment with R-CHOP was associated with significantly better 2-yr (OR 2.9, 95%CI 1.8–4.6) and 5-yr OS (OR 1.8, 95%CI 1.2–2.9) irrespective of race or insurance status.
Previous studies looking at racial differences in treatment of DLBCL showed that black pts present at a younger age,with more advanced disease and were less likely to be treated with combined immunochemotherapy. Our combined institutional study with a large cohort of black pts with DLBCL and detailed ascertainment of prognostic factors and therapy showed that treatment with CHOP is significantly associated with inferior survival in black pts. However, treatment with R-CHOP appears to overcome race as a prognostic factor and is associated with significantly improved survival in all pts subgroups irrespective of race and disease status. This suggests that potential biological differences in DLBCL biology may exist between W & B pts that are no longer prognostic with the addition of rituximab, which we are further exploring with DLBCL subtyping and a study of candidate single nucleotide polymorphisms.
Flowers:Genentech/Biogen-Idec (unpaid): Consultancy; Celgene, Intellikine: Consultancy; Millennium: Research Funding. Foran:GlaxoSmithKline: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal