Abstract
Abstract 1346
Primary central nervous system lymphoma (PCNSL) is a rare extra-nodal non-Hodgkin lymphoma. Outcomes for PCNSL are generally reported to be dismal and the standard of care for treatment remains unclear due to a lack of randomized studies. However, recent studies have demonstrated that intensive chemotherapy with autologous stem cell transplantation (ASCT) is effective as salvage therapy and provides encouraging results as a part of primary therapy. In Alberta, PCNSL is treated exclusively in 2 centres. As one centre adopted ASCT for PCNSL later, we were able to compare the outcomes for patients treated with a strategy including ASCT versus a radiotherapy (RT)-based treatment. We performed a retrospective analysis of the outcomes of all patients diagnosed with PCNSL in Alberta from 1998–2008 to determine the ‘real world’ outcomes for this disease.
Cases of PCNSL were obtained from the Alberta Cancer Board Cancer Registry. Charts were manually reviewed and data extracted on clinical characteristics, treatment, response, toxicities, relapse and survival.
Data was obtained for 95 patients (median age 61) with pathology-confirmed PCNSL of diffuse large B cell lymphoma (DLBCL)-type. Two additional cases with non-DLBCL pathology were excluded from analysis (2 cases with epidural follicular lymphoma and 1 case of marginal zone lymphoma). Eight additional patients were diagnosed with PCNSL by radiology, without pathological confirmation. These patients had a median age of 80 and were uniformly palliated without chemotherapy or RT and were excluded from evaluation. Nine (9.5%) patients were HIV+, of whom 4 were treated with radiotherapy (2 with resultant long-term survival) and 5 were palliated.
Of the HIV- patients, 15 (17%) were treated with palliation alone. These patients had a median age of 70 and only 1 had an ECOG ≤ 1. Twenty-seven patients (34%) were treated with RT alone at a median of 4500cGy. These patients had a median age of 68 and 67% had an ECOG ≥2 at diagnosis. The mean overall survival (OS) for this group was 12 months, similar to previous reports and their 5 year OS was 15%.
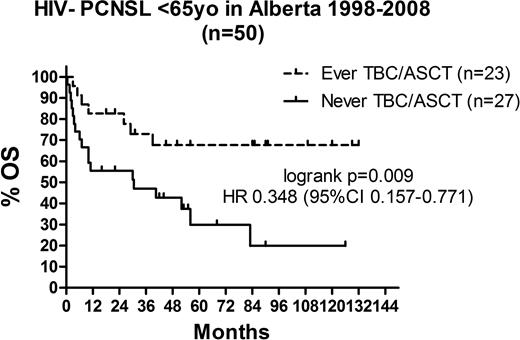
Forty-four patients (46%) were treated with curative intent with therapy including at least one cycle of high-dose methotrexate (HDM). These patients had a median age of 56 and 61% had an ECOG ≥2 at diagnosis. The complete remission (CR) rate, including unconfirmed CR (CRu) was 42%, 38% achieved a partial remission (PR) and 16% were refractory to HDM. Six (13%) received ≤ 3 cycles of HDM, with 2 (4%) early toxic deaths, 2 refractory disease and 2 discontinuations for toxicity. Sixteen (36%) were treated with HDM alone with 14 of these patients receiving ≥ 4 cycles of HDM. Eight patients (18%) were treated with a combination of HDM and RT of which 2 were due to early discontinuation of HDM for progressive disease (1) and toxicity (1). No survival difference was observed for patients treated with HDM alone compared to combined HDM and RT. The median OS for the HDM-treated patients not receiving ASCT as a part of initial therapy was 31 months. Patients <70yrs without major organ dysfunction were offered ASCT if they did not achieve a CR with HDM or later relapsed. All but 3 ASCTs were performed following thiotepa, busulfan and cyclophosphamide (TBC) conditioning. Long-term event-free survival post-ASCT was seen in 11 of 18 patients transplanted in first partial remission, 1 of 3 for patients transplanted for primary refractory/progressive disease, and 5 of 6 patients transplanted for relapsed disease. Three patients died early of transplant-related mortality (TRM). The 5 yr OS of all HIV- PCNSL patients, excluding those receiving only palliation was 37% while the 5 yr OS for patients with PCNSL who received an ASCT (at any time) was 66%. Patients ≤ 65, patients who received an ASCT at any time had a significantly improved survival (5 yr OS 70%) compared to those who did not (5 yr OS 20%). (p=0.009)
ASCT with TBC conditioning is an effective therapy for PCNSL both as a part of primary therapy and for relapsed disease. However, TBC/ASCT is associated with high TRM so efforts should be made to optimize ASCT conditioning to reduce toxicity and make this effective treatment available to more PCNSL patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal