Abstract
Abstract 1343
Multiple myeloma (MM) is the second most common hematological malignancy in the United States with an estimated 20,580 new cases in 2009. Over the past decade, the introduction of novel agents (thalidomide, lenalidomide and bortezomib) have played a pivotal role in improving response rates, duration of response, overall survival (OS) and quality of life. In this study we describe a single center experience with novel agents used for induction followed by high dose chemotherapy (HDT) and first autologous stem cell transplant (ASCT) in patients with MM.
A retrospective review of the medical records of 179 newly diagnosed patients with MM seen between October 2006 and December 2009 at The Ohio State University was performed. All patients received novel therapy containing thalidomide, bortezomib or lenalidomide as part of an induction regimen followed by ASCT. All patients received melphalan 140mg/m2 or 200mg/m2 as preparative regimen. Kaplan-Meier estimates were used to plot progression free survival and overall survival.
Of the 181 patients seen, 2 were excluded because they did not receive a novel agent as part of induction treatment. Of the 179 patients analyzed, median age was 56.8 years (29-80) with 30% of patients older than 60 years. African American represented 19%. Fifty-nine percent were male, 80% had Durie-Salmon (DS) stage III while 25%, 28%, 18% represented International prognostic score (IPS) stage I, II, and III respectively with 27% unknown. Median comorbidity index score was 2 (2-7) and median Karnofsky performance score (KPS) was 90% (70-100).
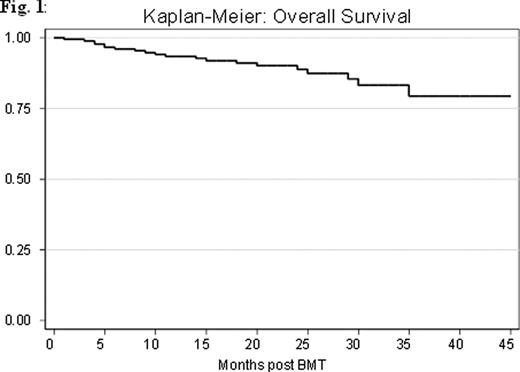
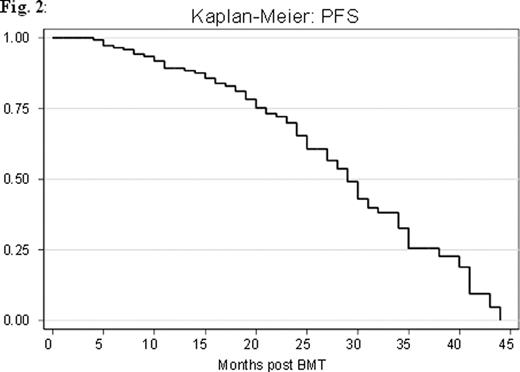
Thirty percent had high risk genetic profile, and 73% received one line of treatment before ASCT. The median time from diagnosis to ASCT was 8.33 months (4-58). The overall response rate (ORR) prior to transplant was 84% (9% complete (CR), 29% very good partial (VGPR), and 46% partial (PR)). The ORR post ASCT was 89% (CR 45%, VGPR 22%, PR 21%). Non relapse mortality was 1% and 3% at 100 days and 1 year respectively. At a median follow up of 31 months (7-90), 69 patients (38%) had relapsed. Median progression free survival (PFS) was 29 months with 1 and 3 years PFS of 79.3% and 61.5% respectively (Fig. 1). The OS was not reached. One and 3 years OS were 93% and 88% respectively (Fig. 1).
Univariate analysis showed that time to transplant > 12 months was associated with poor outcome and decreased overall survival (HR 3.30, p = 0.008). High risk genetic profile was also found to be associated with decreased overall survival although this was not statistically significant (HR 2.31, p = 0.070). Multivariate analysis found that only time to transplant > 12 months was an independent predictor of decreased OS. Significant predictors for disease progression were high risk genetic profile and time to transplant > 12 months in patients receiving 2 or more treatments before ASCT.
Induction with novel agents followed by HDT and ASCT improves CR rate, in our case from 9% to 45%. Median PFS (29 months) was comparable to other published data. OS was not been reached after a median follow up of 31 months. Predictors of progression include high risk genetic profile and time to transplant > 12 months. The only significant predictor for survival was time to transplant. Our study suggests that an early transplant may improve OS and PFS. An extended analysis will be presented at the meeting.
Phillips:NCI/NIH: Research Funding; NCCM Grant: Research Funding; ARRA RC2 Grant: Research Funding. Byrd:Genzyme Corporation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal