Abstract
Abstract 1337
Reduced-intensity conditioning and allogeneic stem cell transplant (RIST), offers an alternative for patients with hematologic malignancies who are not candidates for myeloablative conditioning (MAC) due to the high risk of treatment related toxicity. Despite the reduced “intensity” of RIST preparative regimens, a high incidence of early treatment-related morbidity and mortality persists. The TUFTS regimen represents one such RIST regimen and consists of extracorporeal photopheresis, pentostatin, and reduced dose total body irradiation. The hematopoietic cell transplantation-specific Comorbidity index (HCT-CI) has been reported as an informative predictor of post-transplant survival recipients of fludaribine-based conditioning and SCT, however, its usefulness in patients undergoing allogeneic transplant using alternative conditioning regimens has not been determined. The specific aim of this study was to evaluate the relationship between HCT-CI scores and survival after TUFTS conditioning.
The study employed a retrospective, description design. The sample consisted of adults who underwent allogeneic SCT after a TUFTS preparative regimen at the University of Rochester Medical Center from 2001–2006. Indications for transplant included both myeloid and lymphoid malignancies; recipients of stem cells from either related or unrelated donors, and recipients of prior autologous transplant were also included. The TUFTS conditioning was administered as follows: photopheresis on days -6 and -5, pentostatin 4 mg/m2 on days -4 and -3, reduced dose fractionated total body irradiation to a total of 400–600cGy on days -2 and -1, and SCT on day 0. Sixty-three subjects met the study criteria and we collected study defined and de-identified clinical data from the medical records. Subjects received either tacrolimus and mycophenolate mofetil (MMF) or low-dose methotrexate, or sirolimus and MMF as prophylaxis for graft-versus-host disease. For this study, overall survival (OS) was defined as the time elapsed from date of SCT to the date of death. The HCT-CI score was inclusive of 17 comorbid factors and was calculated for each subject. Total HCT-CI scores were trichotomized three categories; low, intermediate, and high.
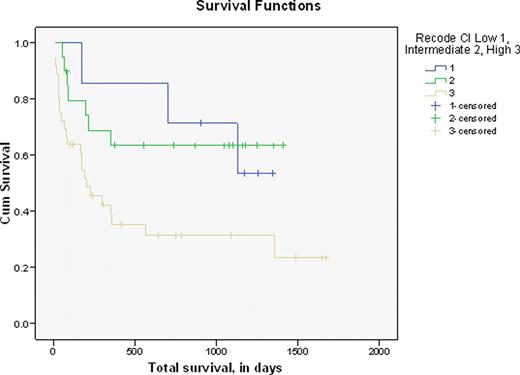
All statistical analyses were performed utilizing SPSS version 15 with an alpha significance set at 0.05. Mean OS was 534.4 days (+/− 515.5). The median survival was 303 days (range 10 to 1673). Subjects were grouped into low (n=7), intermediate (n=20), and high (n=36) HCT-CI score groups. Median survival for each group was 1127, 645, and 181 days, respectively. The Kruskal-Wallis Test was used to evaluate the relationship between trichotomized HCT-CI groups and OS which was re-coded into 6 time-based categories. Mean rank scores for survival were significantly related to HCT-CI categories (p=0.01). A median test on these same variables was also significant where 85.7% (low), 60% (intermediate), and 27.8% (high) of subjects survived to the median survival time point (p=0.004). A Kaplan-Meier survival analysis showed an OS of 46%; HCT-CI group stratification of the survival curve demonstrated that the high CI score group had the lowest survival with a median survival of 202 days (95% CI 64.7, 339.3).
Our findings contribute to the validity of HCT-CI as a valuable instrument for assessing risks that impact survival due to comorbidities in patients conditioned with TUFTS prior to SCT. In this sample, OS was inversely proportional to HCT-CI score and median survival was less than 7 months in the high risk group. To our knowledge, this is the first study that has found a statistically significant correlation between survival and HCT-CI groups in subjects conditioned with TUFTS to treat multiple types of malignancies. We conclude that the HCT-CI assessment should be routinely performed to facilitate decision making with patients who are ineligible for MAC and SCT. This assessment will further add to discussions regarding the risks/benefits of RIST, and decision making with patients in the high risk category who are likely to have low actuarial survival. Further prospective studies are needed to confirm these findings and to evaluate the HCT-CI as a predictor of survival in patients with specific malignancies, different histologic/molecular disease-related factors, varying duration of relapse, and remission status at SCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal