Abstract
Granulysin (GNLY), an antimicrobial protein present in the granules of human cytotoxic T lymphocytes and natural killer (NK) cells, is produced as an intact 15-kDa form that is cleaved to yield a 9-kDa form. Alarmins are endogenous mediators that can induce recruitment and activation of antigen-presenting cells (APCs) and consequently promote the generation of immune response. We hypothesized that GNLY might function as an alarmin. Here, we report that both 9- and 15-kDa forms of recombinant GNLY-induced in vitro chemotaxis and activation of both human and mouse dendritic cells (DCs), recruited inflammatory leucocytes, including APCs in mice, and promoted antigen-specific immune responses upon coadministration with an antigen. GNLY-induced APC recruitment and activation required the presence of Toll-like receptor 4. The observed activity of recombinant GNLY was not due to endotoxin contamination. The capability of the supernatant of GNLY-expressing HuT78 cells to activate DC was blocked by anti-GNLY antibodies. Finally we present evidence that supernatants of degranulated human NK92 or primary NK cells also activated DCs in a GNLY- and Toll-like receptor 4–dependent manner, indicating the physiologic relevance of our findings. Thus, GNLY is the first identified lymphocyte-derived alarmin capable of promoting APC recruitment, activation, and antigen-specific immune response.
Introduction
The granulysin (GNLY) gene is located on chromosome 2 and consists of 6 exons. A major protein product of 15 kDa is translated, some of which is subsequently secreted or processed by proteolytic cleavage at both N and C termini to a 9-kDa protein stored in the granular compartment.1 Whereas the 15-kDa protein is produced rapidly, has a shorter half-life, and is constitutively released, the secretory 9-kDa form is produced slowly and is relatively stable. The crystal structure of the human protein, elucidated in 2003 by Anderson et al, is predictive of its antimicrobial effects and clinical relevance in disease and pathogenesis. GNLY is highly cationic and folded as a 5-helix bundle stabilized by 2 highly conserved intramolecular disulfide bonds.2 It belongs to the family of Saposin-like lipid binding proteins called SAPLIP and colocalizes in the granular compartments of cytotoxic T lymphocytes (CTLs) and natural killer (NK) cells along with granzymes and perforin.3 GNLY has the highest sequence identity to NK-lysin (43% identity), a porcine protein with antibacterial activity that is also a member of the SAPLIP family.3 No homologous protein has been identified to date in mice.
GNLY is produced by human NK cells and activated CTLs, and the 9-kDa form is rapidly released upon degranulation. The kinetics of expression of GNLY by these 2 cell types differs. NK cells release GNLY very early in immune responses, whereas CTLs release it after 3-5 days of activation.1 Elevation of GNLY expression and levels in tissue and serum has been reported in infections, autoimmune diseases, transplant rejection, and graft versus host reaction in patients with hematopoietic stem cell transplantation.4-10 In leprosy, CD4+ cells expressing GNLY were elevated (8%-15%) in the skin lesions of patients with the tuberculoid form compared with those with the disseminated lepromatous form of the disease.7 Recent studies have demonstrated that in response to Mycobacterium tuberculosis–infected macrophages, human CD8+ T cells were induced to express CCL5 and GNLY.11 Recently, it was reported that blister fluids of patients suffering from Stevens Johnson syndrome and toxic epidermal necrolysis contained high levels of secretory 15-kDa GNLY, and the high concentration of GNLY, but not granzyme B or perforin, is responsible for the disseminated keratinocyte apoptosis in Stevens Johnson syndrome and toxic epidermal necrolysis.12 By contrast, patients with severe immunodeficiencies have very low GNLY serum levels.13 GNLY levels are also reduced in different cell types and even in serum of carcinoma patients and appear to be inversely correlated with tumor progression.14-17 Consequently both forms of GNLY can be induced in the course of inflammation and have also been shown to be up-regulated by stimulation of lymphoid cells by proinflammatory mediators and pathogen-associated molecular patterns.18,19
GNLY exhibits lytic activity against a variety of microorganisms and tumors.3,14,20-22 It binds to a variety of lipids, including cholesterol and sphingolipids, and damages microbial cell membranes by binding to negatively charged molecules.23 In addition to its antimicrobial effects, GNLY is also cytolytic for various tumor cells by disrupting the transmembrane potential (Δc) in the mitochondria, resulting in release of cytochrome c and apoptosis by activation of caspase 3.24-26
We have been investigating the immunostimulating effects of various endogenous antimicrobial peptides and proteins including defensins, cathelicidin, eosinophil-derived neurotoxin, high mobility group box proteins, and lactoferrin. Based on their interactions with host cells, these molecules are important mobilizers and activators of innate inflammatory responses and promote antigen specific adaptive immune responses when coadministered with antigen in vivo.27-31 We classified them as alarmins based on their capacity to recruit and activate antigen-presenting cells (APCs). Recently it was shown that at nanomolar concentrations recombinant 9-kDa GNLY chemoattracted monocytes, mature dendritic cells (DCs), NK cells, and T cells and at micromolar concentrations induced the production of certain inflammatory mediators by monocytic cell lines.32 Together with the finding that mice expressing transgenic human GNLY were more resistant to tumor challenge,33 we speculated that GNLY might act as an alarmin. Therefore, we investigated the effects of GNLY on APCs and antigen-specific immune response and dissected the underlying mechanism(s). We show here that both the 9- and 15-kDa forms of GNLY are chemotactic in vitro and induce the recruitment of leukocytes including APCs in vivo. GNLY activates mouse and human DCs and promotes antigen-specific immune responses in a Toll-like receptor 4 (TLR4)–dependent manner. Thus, GNLY exhibits the characteristics of an alarmin and is the first lymphocyte-derived alarmin to be identified.
Methods
Mice and reagents
Female wild-type (wt) C57BL/6 mice, 6 to 8 weeks old, were provided by the Animal Production Facility of the NCI. NCI is approved by the American Association for the Accreditation of Laboratory Animal Care International and follows the Public Health Service policy for the Care and Use of Laboratory Animals. Animal care was provided in accordance with the procedures outlined in the Guide for Care and Use of Laboratory Animals (National Research Council, Washington, DC). Human recombinant (r) granulocyte macrophage colony-stimulating factor (GM-CSF), interleukin-4 (IL-4), and RANTES/CCL5 were purchased from PeproTech. Bovine serum albumin, pertussis toxin (PTx), fluorescein isothiocyanate (FITC)-conjugated goat antimouse immunoglobulin G (IgG), strontium chloride, and β-mercaptoethanol were from Sigma. 3H-TdR was purchased from NEN. RPMI 1640, glutamine, penicillin, streptomycin, and HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid) were from BioWhittaker. Fetal bovine serum (FBS) was purchased from Hyclone. Ultrapure lipopolysaccharide (LPS) was purchased from Invivogen. All antibodies used for flow cytometry analysis were purchased from BD/Pharmingen, including FITC-conjugated mouse anti–human CD83, FITC-conjugated mouse anti–human CD80, phycoerythrin (PE)-conjugated mouse anti–human CD86, PE-conjugated mouse anti–human HLA-DR, as well as FITC- and/or PE-conjugated, isotype-matched mouse IgG1, κ, IgG2a, κ, and IgG2b. GNLY (9-kDa) was prepared and purified as described previously.32 Contamination of GNLY with endotoxin was assessed using the Limulus amebocyte lysate assay (Sigma-Aldrich). Endotoxin contamination was < 1.0 EU/μg GNLY. Recombinant GNLY (15 kDa) was purchased from R&D Systems. Anti-TLR4 antibodies were purchased from eBioscience.
Cell culture
Human peripheral blood enriched in mononuclear cells was obtained from healthy donors by leukopheresis30,31 (Transfusion Medicine Department, Clinical Center, National Institutes of Health, Bethesda, MD, with an approved human subject's agreement). The enriched monocyte populations obtained after gradient centrifugation were used for further experiments. Monocyte-derived immature DC (Mo-iDC) were generated as described previously.31 Subsequently, DCs were incubated in fresh G4 (RPMI 1640 plus 10% FBS plus 50 ng/mL GM-CSF and IL-4) medium in the absence or presence of GNLY or LPS at the specified concentrations for 24-48 hours in a CO2 (5%) incubator. For certain experiments, fresh peripheral blood–derived CD1c positive DCs were purified using a CD1c (BDCA-1) plus Dendritic Cell Isolation Kit (Miltenyi Biotec). Purified cells were 95%-98% CD1c+. For some experiments, primary NK cells were isolated from human peripheral blood using a CD56+CD16+ NK cell isolation kit (Miltenyi Biotec). Monocytes from the same donor were used to generate Mo-iDC as described previously. The NK-92 cell line was a gift from Dr Steve Anderson (LEI, CIP, NCI, Frederick, MD) and was maintained in RPMI 1640 with 10% FBS supplemented with 1000 U recombinant hIL2, 50μM β-mercaptoethanol, and minimum essential medium nonessential amino acids.
Chemotaxis assay
DC migration was assessed using a 48-well microchemotaxis chamber as described previously.31 GNLY and other proteins were diluted with chemotaxis medium (RPMI 1640 plus 1% bovine serum albumin). Different concentrations of putative chemotactic factors were placed in wells of the lower compartment of the chamber (Neuro Probe), and the DC suspension (1 × 106 cells/mL) was added in wells of the upper compartment. To investigate the effect of pertussis toxin on migration, monocyte-derived DC (Mo-DC) were pretreated with 100 ng/mL pertussis toxin for 30 minutes at 37°C before chemotaxis assays. The lower and upper compartments were separated by a 5-μm polycarbonate filter (Osmonics). After incubation at 37°C for 1.5 hours in humidified air with 5% CO2, the filters were removed and stained, and the cells that had migrated across the filter were counted with the use of a Bioquant Life Science counting software (Bioquant Image Analysis Corp). The results are presented as the number of migrating cells per high-power field (No./HPF).
Treatments, neutralization, and blocking experiments
For activation experiments, DCs were treated with different doses of recombinant GNLY (both 9- and 15-kDa forms) or ultrapure Escherichia coli K12 LPS at 1 μg/mL (Invivogen) for 36-48 hours as indicated. For some experiments, different concentrations of supernatants from degranulated NK cells or transfected HuT cells were tested for 48 hours at 37°C. For blocking TLR4, DCs were treated with 10 μg of monoclonal antibody (mAb) antiTLR4 (eBioscience) for 1 hour before treatments with various stimuli. mAb IgG1 and IgG2b (eBioscience) were used as isotype controls. Neutralization of GNLY was performed by incubating the recombinant protein with mAb DH10 for 30 minutes at 37°C.21 GNLY in supernatants was depleted by immunoprecipiation using protein G Dynabeads (Invitrogen) as per the manufacturer's protocol. Briefly 10 μg bound anti-GNLY (DH10) was incubated with 100-200 μL of degranulated supernatants and gently rotated for 45 minutes. Supernatants were depleted of GNLY by magnetic separation and the process was repeated twice.
Mixed lymphocyte reaction
Allogeneic mixed lymphocyte reaction (MLR) was performed as described.31 Briefly, purified, allogeneic T cells (105/well) were cultured with different numbers of DCs in a 96-well, round-bottom plate for 5 days at 37°C in humidified air with 5% CO2. The proliferative response of T cells was examined by pulsing the culture with 3H-TdR (0.5 μCi/well) for the last 18 hours before harvesting. 3H-TdR incorporation was measured with a microβ counter (Wallace).
In vivo recruitment of leukocytes
C57BL/6NCr mice (6-8 weeks old) were injected intraperitoneally with 1.0 mL of phosphate-buffered saline (PBS) containing 10 μg/mL of 9-kDa GNLY or 1 μg/mL LPS. Control mice received PBS alone. Mice were killed after 4 and 24 hours, and cells were harvested by peritoneal lavage using 5 mL of ice-cold PBS supplemented with 5mM EDTA (ethylenediaminetetraacetic acid) and 20 U/mL heparin. Cells were counted, and their surface phenotype was determined using a FACSort flow cytometer (BD Biosciences).
Generation of mouse DCs
DCs were generated from the bone marrow of C57BL6 or C3H/HeJ or C3H/HeN mice according to the methods of Inaba et al with minor modification.34 Briefly, red blood cell-depleted bone marrow cells isolated from femurs and tibia were plated in 6-well tissue culture plates in complete RPMI 1640 medium supplemented with mGM-CSF (25 ng/mL). After 48 hours of incubation, nonadherent cells were discarded, and fresh medium containing GM-CSF was added. The cells were cultured for additional 48 hours and washed to remove nonadherent cells and supplemented with fresh complete medium with GM-CSF as before. On day 6, nonadherent cells (more than 95% were CD11c-positive) were collected and used as mouse bone marrow–derived iDC for chemotaxis and activation experiments. Subsequently, DCs were incubated in fresh medium in the absence or presence of GNLY or LPS at specified concentrations for 24-48 hours in a CO2 (5%) incubator before analysis of their expression of surface markers, production of cytokines in the culture supernatants.
Induction of antigen-specific humoral- and cell-mediated responses
Eight-week-old C57BL/6 or C3H HeN or C3H/HeJ mice (4 mice/group) were injected intraperitoneally on day 1 with 0.2 mL PBS containing 50 μg of ovalbumin (OVA) in the presence or absence of alum or 15-kDa GNLY (20 μg/mouse). Mice were boosted after 7 days with OVA alone, or OVA and GNLY, or OVA and alum. Two days later, mice were euthanized, and spleen cells were analyzed for antigen-specific cell–mediated responses. Cells from individual spleens were analyzed either by proliferation assays and cytokine production.
OVA-specific splenocyte proliferation and/or cytokine production were measured as previously described with minor modifications.32 Briefly, splenocytes (5 × 105/well) were seeded in triplicate in wells of round-bottomed 96-well plates in complete RPMI 1640 medium (0.2 mL/well) and incubated in the presence or absence of indicated concentration of OVA at 37°C in a CO2 incubator for 72 hours. The cells were pulsed with 3H-TdR (0.5 μCi/well) for the last 18 hours to assess splenocyte proliferation. Alternatively, pooled splenocytes of each group were cultured in complete RPMI 1640 in 24-well plates (5 × 106/1 mL/well) with indicated concentrations of OVA for 48 hours before the culture supernatants were harvested to determine their cytokine content (Aushon Biosciences).
Degranulation assays
For release of cytotoxic granules, both NK92 cells and fresh NK cells were treated with 25mM SrCl2 for 18-24 hours. Cells were cultured at a concentration of 2 × 106 cells/mL in RPMI 1640 with 10% FBS or in AIM V medium supplemented with 2000 U recombinant hIL2, 50μM β-mercaptoethanol, and minimum essential medium nonessential amino acids. Supernatants were concentrated and dialyzed 3 times (to remove residual Strontium) with RPMI 1640 using Amicon Ultra-4 Centrifugal Filter Unit with Ultracel-3 membrane (Millipore). Samples were adjusted to one-tenth the starting volume and filter-sterilized using 0.2-μm filters (Millipore) and frozen. For DC activation, supernatants were added to DC cultures (autologous in case of primary NK supernatants) at a final concentration of 1%-10%.
Statistical analysis
Data were analyzed using paired 2-tailed Student t test or Mann Whitney test comparing untreated samples with GNLY-treated or LPS-treated samples. Certain experiments were analyzed using 2-way analysis of variance comparing responses between different groups using GraphPad Prism software Version 5 (GraphPad).
Results
Granulysin chemoattracts immature DCs in vitro
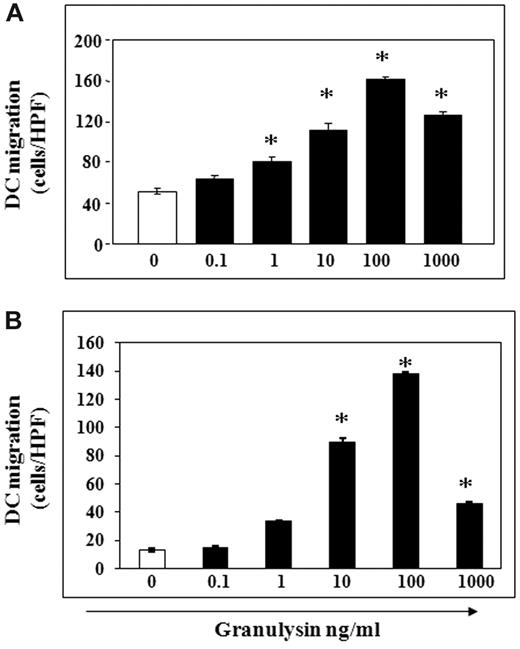
In the course of inflammation either in response to tissue damage or infection, DC precursors and DCs are recruited to the inflamed tissue where they capture and process antigen before they mature and traffic to secondary lymphoid organs. To determine whether GNLY could recruit APCs, we first tested whether GNLY was chemotactic for human Mo-DCs and mouse bone marrow-derived DCs (BMDCs). Both 9-kDa (recombinant protein produced in E coli) and 15-kDa (recombinant protein produced in mammalian cells) of GNLY were tested. Using a modified Boyden chamber assay, we observed that GNLY (9-kDa form) consistently induced the migration of Mo-iDC in a dose-dependent manner with a peak response at 100 ng/mL (Figure 1A). To further investigate whether GNLY-induced migration of Mo-iDC was mediated by a Gi protein–coupled receptor, Mo-iDC were pretreated with PTx. Pretreatment with nontoxic doses of PTx inhibited the migration induced by GNLY (supplemental Figure 1A, available on the Blood Web site; see the Supplemental Materials link at the top of the online article), indicating that the chemotactic effect of GNLY on immature DCs was mediated by a Gi protein-coupled receptor. GNLY-induced migration was also inhibited when an equal concentration of the protein was added to both wells, indicating that GNLY-induced DC migration was chemotactic rather than chemokinetic (supplemental Figure 1B). The identity of the chemotactic receptor remains to be established. Although, no murine ortholog of GNLY has been reported to date, the 9-kDa form of GNLY also induced the migration of day 6 mouse BMDCs in a dose-dependent manner, indicating that human GNLY was chemotactic for murine cells (Figure 1B). This effect was probably mediated through GNLY responsive receptors in mice. Similar results were observed with the 15-kDa form of GNLY (data not shown).
Granulysin induces chemotactic migration of iDCs. Chemotactic effect of 9-kDa GNLY on human Mo-iDC and mouse BMDC were assessed as described in “Chemotaxis assay.” (A) Chemotactic effect of 9-kDa GNLY on human Mo-iDC. (B) Chemotactic effect of 9-kDa GNLY on mouse BMDCs. No./HPF indicates the average number of cells per high-powered field. Mean ± SD; *P < .05. Triplicate wells are shown; 1 representative experiment of 3 is shown.
Granulysin induces chemotactic migration of iDCs. Chemotactic effect of 9-kDa GNLY on human Mo-iDC and mouse BMDC were assessed as described in “Chemotaxis assay.” (A) Chemotactic effect of 9-kDa GNLY on human Mo-iDC. (B) Chemotactic effect of 9-kDa GNLY on mouse BMDCs. No./HPF indicates the average number of cells per high-powered field. Mean ± SD; *P < .05. Triplicate wells are shown; 1 representative experiment of 3 is shown.
Granulysin recruits murine leukocytes in vivo
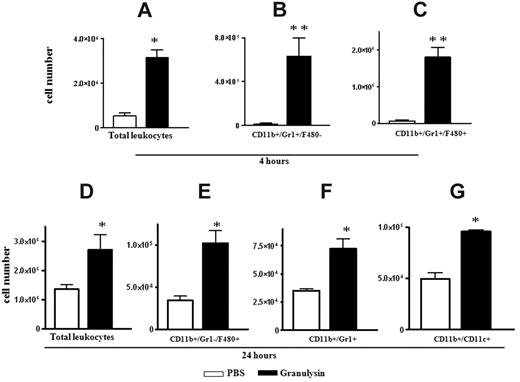
To determine whether human recombinant GNLY could also recruit mouse inflammatory cells in vivo; 9-kDa GNLY was injected into the peritoneal cavity of C57BL/6 mice. Peritoneal lavage obtained 4 or 24 hours later showed that GNLY induced a substantial increase in intraperitoneal inflammatory leukocytes compared with PBS-injected mice at both 4 hours (P ≤ .05; Figure 2A) and 24 hours (P ≤ .05; Figure 2D). The major populations of cells recruited after 4 hours were CD11b+/Gr1+/F4/80neg neutrophils (P ≤ .01; Figure 2B) and CD11b+/Gr1+/F4/80+ inflammatory monocytes (P ≤ .01; Figure 2C). However, after 24 hours, the inflammatory monocytes were replaced by a subpopulation of Gr1neg/F4/80+ macrophages (P ≤ .05; Figure 2E). Other cells recruited were neutrophils and myeloid CD11b+/CD11c+ DCs (P ≤ .05; Figure 2F-G).
Granulysin recruits leukocytes in vivo. For in vivo recruitment experiments C57BL mice were injected intraperitoneally with PBS or 10 μg/mouse of 9-kDa GNLY (4 mice per group). Mice were killed, and the peritoneal cavity was rinsed with 5 mL of cold PBS, 5mM EDTA, 20 U/mL heparin. Cells in the peritoneal lavage were counted and stained to analyze the phenotype of the recruited cells by flow cytometric analysis after 4 hours of injection: (A) total number of cells, (B) CD11b/Gr1+/F480+, (C) CD11b/Gr1+/F480−, and at 24 hours (D) total number of cells, (E) CD11b/Gr1−/F480+, (F) CD11b/Gr1+/F480−, and (G) CD11b+/CD11c+. One representative experiment of 3 is shown. *P < .05, **P < .01.
Granulysin recruits leukocytes in vivo. For in vivo recruitment experiments C57BL mice were injected intraperitoneally with PBS or 10 μg/mouse of 9-kDa GNLY (4 mice per group). Mice were killed, and the peritoneal cavity was rinsed with 5 mL of cold PBS, 5mM EDTA, 20 U/mL heparin. Cells in the peritoneal lavage were counted and stained to analyze the phenotype of the recruited cells by flow cytometric analysis after 4 hours of injection: (A) total number of cells, (B) CD11b/Gr1+/F480+, (C) CD11b/Gr1+/F480−, and at 24 hours (D) total number of cells, (E) CD11b/Gr1−/F480+, (F) CD11b/Gr1+/F480−, and (G) CD11b+/CD11c+. One representative experiment of 3 is shown. *P < .05, **P < .01.
Granulysin induces phenotypic and functional maturation of human Mo-DC and peripheral blood dendritic cells
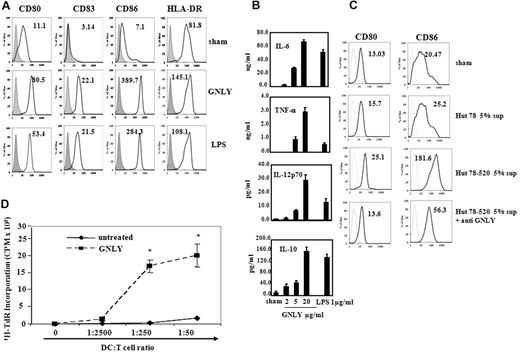
The previously reported activation of human monocytes by GNLY led us to speculate that GNLY might be an activator of myeloid DCs. Fully activated DCs acquire a mature phenotype, characterized by up-regulation of certain costimulatory and major histocompatibility complex molecules, production of a variety of inflammatory cytokines and chemokines, and enhancement of antigen-presenting capacity. To determine whether GNLY could activate DCs, we treated both human Mo-DC as well as CD1c+ peripheral blood DCs for approximately 24-48 hours. Dose response studies showed that 20 μg/mL of both 9-kDa and 15-kDa GNLY were able to up-regulate DC expression of surface markers like CD80, CD83, CD86, and major histocompatibility complex class II within 48 hours, indicating that these DCs acquired phenotypic markers of maturation (Figure 3A and supplemental Figure 2A). GNLY-treated DCs also produced high levels of IL-6, IL-8, IL-12, IL-10, and tumor necrosis factor α (TNFα; Figure 3B and supplemental Figure 2B). There was also a marked increase in the production of the chemokines MCP1 and MDC (data not shown). We also analyzed the effect of 9-kDa GNLY on freshly isolated human peripheral blood myeloid CD1c+ DCs. Within 36 hours, GNLY-treated peripheral blood myeloid CD1c+ DCs produced high amounts of proinflammatory cytokines such as IL-1β, IL-6, IL-8, TNFα, and IL-12 compared with untreated cells (supplemental Figure 3). We also observed that 15-kDa GNLY was much more potent than the 9-kDa form in promoting DC activation as assessed by the production of a proinflammatory cytokine like IL-6 (supplemental Figure 2C). In addition, complete DC maturation was observed at 2-10 μg/mL range of the 15-kDa form. Therefore, the 15-kDa form (10 μg/mL) was used for all the subsequent in vitro DC activation experiments. To further confirm whether DC activation was specifically due to GNLY, we tested supernatants from HuT78, a human T-cell tumor line that does not possess cytotoxic granules, and HuT78 cells transfected with 520 cDNA (HuT78-520) expressing mainly the 15-kDa form of GNLY on DC cultures.21 We observed that even at a final concentration of 1%-2%, supernatants from HuT78-520 but not HuT78, were able to induce phenotypic maturation of DCs (data not shown), and this effect was diminished when the supernatants were treated with anti-GNLY antibodies before addition to the DC culture (Figure 3C).
Granulysin activates human Mo-iDCs. Mo-iDCs were cultured at 1 × 106 cells/mL in the presence or absence of 10 μg/mL 15-kDa GNLY and 1 μg/mL ultrapure LPS for 48 hours. Cells were then analyzed for (A) expression of costimulatory molecules on Mo-DC by fluorescence-activated cell sorting (FACS) and (B) production of cytokines by Mo-DC. To further confirm whether DC activation was specifically due to GNLY, Hut-78 (WT) or Hut 78-520 (transfected with 15 kDa GNLY cDNA) cells were cultured at 2 × 106/mL in complete RPMI 1640 for 48 hours. Cells were centrifuged, and supernatants collected. Mo-iDCs were treated with 5% of supernatants in the presence or absence of anti-GNLY (C). Cells were then analyzed for expression of costimulatory molecules on Mo-DC by FACS. Gray lines represent isotype control. Data are shown as geometric mean fluorescence of intensity. One representative experiment of 4 is shown. To assess functional activation of DCs by 15-kDa GNLY, proliferation of allogeneic, human peripheral blood T lymphocytes by GNLY-treated Mo-DCs were compared with that of untreated DCs (D). T cells (105/well) were cultured in triplicate in the absence or presence of DCs at the concentrations specified in 96-well plates for 6 days with the addition of 3H-TdR (0.5 μCi/well) in the last 18 hours of incubation. The cells were harvested and measured for the incorporation of 3H-TdR (mean ± SD). DCs were treated with or without (untreated) 10 μg/mL 15-kDa GNLY for 48 hours at 37°C in humidified air with 5% CO2 before use in the allogeneic MLR experiments. **P < .001. One representative experiment of 3 is shown.
Granulysin activates human Mo-iDCs. Mo-iDCs were cultured at 1 × 106 cells/mL in the presence or absence of 10 μg/mL 15-kDa GNLY and 1 μg/mL ultrapure LPS for 48 hours. Cells were then analyzed for (A) expression of costimulatory molecules on Mo-DC by fluorescence-activated cell sorting (FACS) and (B) production of cytokines by Mo-DC. To further confirm whether DC activation was specifically due to GNLY, Hut-78 (WT) or Hut 78-520 (transfected with 15 kDa GNLY cDNA) cells were cultured at 2 × 106/mL in complete RPMI 1640 for 48 hours. Cells were centrifuged, and supernatants collected. Mo-iDCs were treated with 5% of supernatants in the presence or absence of anti-GNLY (C). Cells were then analyzed for expression of costimulatory molecules on Mo-DC by FACS. Gray lines represent isotype control. Data are shown as geometric mean fluorescence of intensity. One representative experiment of 4 is shown. To assess functional activation of DCs by 15-kDa GNLY, proliferation of allogeneic, human peripheral blood T lymphocytes by GNLY-treated Mo-DCs were compared with that of untreated DCs (D). T cells (105/well) were cultured in triplicate in the absence or presence of DCs at the concentrations specified in 96-well plates for 6 days with the addition of 3H-TdR (0.5 μCi/well) in the last 18 hours of incubation. The cells were harvested and measured for the incorporation of 3H-TdR (mean ± SD). DCs were treated with or without (untreated) 10 μg/mL 15-kDa GNLY for 48 hours at 37°C in humidified air with 5% CO2 before use in the allogeneic MLR experiments. **P < .001. One representative experiment of 3 is shown.
To further determine whether GNLY-induced DC maturation was reflected at the functional level, GNLY-treated Mo-DCs were analyzed for their capacity to stimulate the proliferation of allogeneic T cells at various DC:T cell ratios in an allogeneic MLR assay. GNLY-treated DCs stimulated the proliferation of allogeneic T cells at a DC:T cell ratio greater that 1:2500, demonstrating their remarkably enhanced capacity for presenting antigen to T cells compared with Mo-iDC that had not been stimulated by GNLY (Figure 3D). Hence, GNLY clearly can induce both phenotypic and functional maturation of myeloid DCs, which is necessary for the initiation of adaptive immune responses.
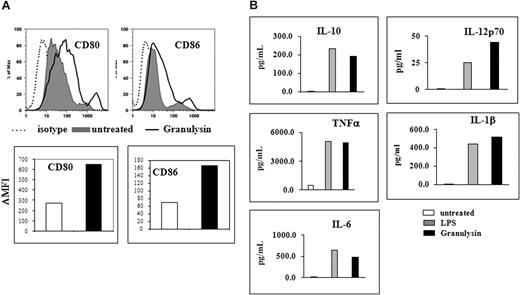
Granulysin activates mouse BMDCs
GNLY was chemotactic for both mouse and human DCs in vitro and recruited leukocytes in vivo in mice, indicating that it probably interacts with similar chemotactic receptors on both human and mouse cells. To further analyze whether GNLY could activate mouse DCs, we treated BMDCs from C57BL/6 mice with 10 μg/mL 15-kDa GNLY and assessed cell-surface phenotype and production of proinflammatory cytokines after 48 hours. Human GNLY caused increased expression of CD80 and CD86 (Figure 4A) and cytokines including IL-6, IL-10, IL-12, and TNFα (Figure 4B), indicating that GNLY is also a potent activator for mouse DCs.
Granulysin activates mouse BMDCs. BMDCs were cultured at 1 × 106 cells/mL in the presence or absence of 15-kDa GNLY at a concentration of 10 μg/mL and 1 μg/mL ultrapure LPS for 48 hours. Shown are the phenotypic expression of CD80 analyzed by FACS (A) and production of cytokines by BMDCs (B). One representative experiment of 4 is shown.
Granulysin activates mouse BMDCs. BMDCs were cultured at 1 × 106 cells/mL in the presence or absence of 15-kDa GNLY at a concentration of 10 μg/mL and 1 μg/mL ultrapure LPS for 48 hours. Shown are the phenotypic expression of CD80 analyzed by FACS (A) and production of cytokines by BMDCs (B). One representative experiment of 4 is shown.
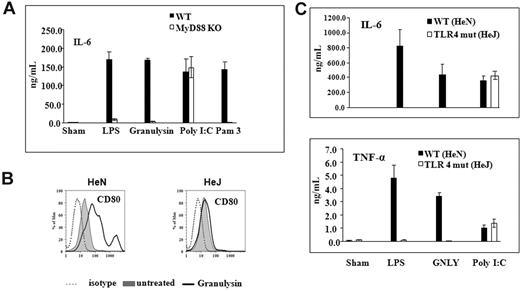
Granulysin activation of APCs is MyD88-dependent and requires TLR4
The fact that GNLY acts as a proinflammatory mediator for both human and mouse cells led us to investigate its putative activating receptor. We first examined the involvement of MyD88 using 2 murine macrophage cell lines derived from MyD88+/+ or littermate-matched MyD88−/− B6/129 mice, respectively. Both wild-type and MyD88 KO macrophages were treated with the 15-kDa form of GNLY for 24 hours, and supernatants were assayed for IL-6. As shown in Figure 5A, both GNLY and Pam3-Cys, an agonist for TLR1/2, induced IL-6 production by wild-type macrophages. In contrast, neither GNLY nor Pam3 induced IL-6 production by MyD88 KO macrophages. The lack of IL-6 production by MyD88 KO macrophages in response to GNLY or Pam3 was not due to an intrinsic inability of the cells to generate IL-6, because they produced similar level of IL-6 in response to poly I:C, a ligand for TLR3 that signals through TRIF, but not MyD88. Therefore, GNLY-induced activation of APCs was dependent on MyD88.
Granulysin activation of APCs is MyD88-dependent and requires TLR4. (A) Mouse macrophage cells from WT B6129 or B6 MyD88-deficient cells lines (MyD88 KO) were incubated at 106/mL in the presence of 10 μg/mL 15-kDa GNLY, 1 μg/mL Pam3, 1 μg/mL ultrapure LPS, or 5 μg/mL poly I:C for 48 hours, and the production of IL-6 in the culture supernatants was measured by enzyme-linked immunosorbent assay. The results of 1 experiment representative of 2 are presented as the average (mean ± SD) of triplicate wells. To analyze the role of TLR4 in GNLY-mediated activation, day 6 mouse BMDCs from WT (HeN) and TLR4 mutant (HeJ) mice were incubated at 106/mL in the presence of 10 μg/mL 15-kDa GNLY and 1 μg/mL ultrapure LPS for 48 hours. After treatment, cells were analyzed by FACS for induction of costimulatory molecules and production of proinflammtory cytokines in the culture supernatants by enzyme-linked immunosorbent assay. (B) Analysis of CD80 and CD86 surface markers compared between untreated and GNLY-treated cells. (C) Induction of proinflammatory cytokines by GNLY compared with untreated and LPS (positive control). One representative experiment of 4 is shown. *P < .01.
Granulysin activation of APCs is MyD88-dependent and requires TLR4. (A) Mouse macrophage cells from WT B6129 or B6 MyD88-deficient cells lines (MyD88 KO) were incubated at 106/mL in the presence of 10 μg/mL 15-kDa GNLY, 1 μg/mL Pam3, 1 μg/mL ultrapure LPS, or 5 μg/mL poly I:C for 48 hours, and the production of IL-6 in the culture supernatants was measured by enzyme-linked immunosorbent assay. The results of 1 experiment representative of 2 are presented as the average (mean ± SD) of triplicate wells. To analyze the role of TLR4 in GNLY-mediated activation, day 6 mouse BMDCs from WT (HeN) and TLR4 mutant (HeJ) mice were incubated at 106/mL in the presence of 10 μg/mL 15-kDa GNLY and 1 μg/mL ultrapure LPS for 48 hours. After treatment, cells were analyzed by FACS for induction of costimulatory molecules and production of proinflammtory cytokines in the culture supernatants by enzyme-linked immunosorbent assay. (B) Analysis of CD80 and CD86 surface markers compared between untreated and GNLY-treated cells. (C) Induction of proinflammatory cytokines by GNLY compared with untreated and LPS (positive control). One representative experiment of 4 is shown. *P < .01.
To investigate the possibility that GNLY might act as an endogenous ligand for one of the TLRs, we first isolated BMDC from TLR4 mutant mice C3H/HeJ (harboring a point mutation that renders TLR4 nonfunctional) and wild-type C3H/HeN mice. GNLY-treated C3H/HeN DC acquired a mature phenotype with up-regulation of CD80 (Figure 5B) and production of proinflammatory cytokines like IL-6 and TNFα (Figure 5C). In contrast, GNLY-treated C3H/HeJ DC failed to up-regulate cell surface makers and did not produce proinflammatory cyto-kines (Figure 5B-C). Thus, the activating effect of GNLY was mediated by TLR4.
Granulysin acts as an adjuvant and requires intact TLR4 for mediating adaptive immune responses
The finding that GNLY could induce simultaneous recruitment and activation of various APCs through TLR4 in vitro prompted us to investigate whether GNLY possessed an in vivo immunoenhancing adjuvant activity and whether this effect required functional TLR4. For these studies, we used both the 15-kDa and 9-kDa forms of GNLY. C57BL/6 or C3H HeN or TLR4 mutant C3H/HeJ mice were immunized with OVA in the presence or absence of GNLY, using alum as a positive control. Mice were boosted either after 1 week with OVA in the presence or absence of GNLY or alum and euthanized 2 days later. For some experiments booster was given at 2 weeks, and mice were euthanized 1 week later. Splenocytes from either C3H/HeN or C57/Bl6 mice immunized with OVA plus GNLY exhibited more robust proliferation in response to OVA stimulation than that of splenocytes of mice immunized with OVA alone (Figure 6A and supplemental Figure 4A, respectively). In addition, splenocytes of mice from these 2 strains immunized with OVA plus GNLY also produced higher levels of Th1 and Th2 cytokines upon OVA stimulation than mice immunized with OVA alone (Figure 6B and supplemental Figure 4B). On the contrary, the adjuvant activity of GNLY was lost in TLR4 loss-of-function HeJ mice as seen in Figure 6A-B.
Granulysin-mediated cognate immune responses are hampered in TLR4 mutant mice. C3H/HeN and HeJ mice (4 mice per group) were injected intraperitoneally either with 50 μg of OVA alone or with 15-kDa GNLY (20 μg/mouse) or alum. One week later, mice were boosted with the same combination. After 2 days, mice were killed, and the ability to induce OVA-specific splenocyte proliferation (A) and cytokine production (B) was measured. Splenocytes from individual spleens from each group (5 × 105/0.2 mL/well) were stimulated with 50 μg/mL OVA for 72 hours with [3H]-TdR pulse (0.5 μCi/well) for the last 18 hours. For cytokine measurement, (1 × 106/0.2 mL/well) cells from individual spleen were plated with 50 μg/mL OVA, and supernatants were collected after 72 hours. Splenocyte proliferation (mean ± SD) [3H]-TdR incorporation (counts per minute) of triplicate wells and cytokine production from individual mice of 1 experiment representative of 2 are shown. *P < .01, **P < .001, ***P < .0005. ns, not significant.
Granulysin-mediated cognate immune responses are hampered in TLR4 mutant mice. C3H/HeN and HeJ mice (4 mice per group) were injected intraperitoneally either with 50 μg of OVA alone or with 15-kDa GNLY (20 μg/mouse) or alum. One week later, mice were boosted with the same combination. After 2 days, mice were killed, and the ability to induce OVA-specific splenocyte proliferation (A) and cytokine production (B) was measured. Splenocytes from individual spleens from each group (5 × 105/0.2 mL/well) were stimulated with 50 μg/mL OVA for 72 hours with [3H]-TdR pulse (0.5 μCi/well) for the last 18 hours. For cytokine measurement, (1 × 106/0.2 mL/well) cells from individual spleen were plated with 50 μg/mL OVA, and supernatants were collected after 72 hours. Splenocyte proliferation (mean ± SD) [3H]-TdR incorporation (counts per minute) of triplicate wells and cytokine production from individual mice of 1 experiment representative of 2 are shown. *P < .01, **P < .001, ***P < .0005. ns, not significant.
Furthermore, OVA plus GNLY immunized mice showed a 10-fold increase in serum anti-OVA antibody titer compared with mice immunized with OVA alone (supplemental Figure 4C). These data indicated that GNLY enhanced OVA-specific cellular and humoral immune responses and had adjuvant activity that required intact TLR4 to generate adaptive immune responses. Of note, GNLY induced higher levels of interferonγ and lower levels of IL-4 and IL-5, suggesting that it favors Th1 polarization compared with alum that favors Th2 responses. Thus, human GNLY augmented antigen specific responses and acted as an adjuvant and alarmin in vivo.
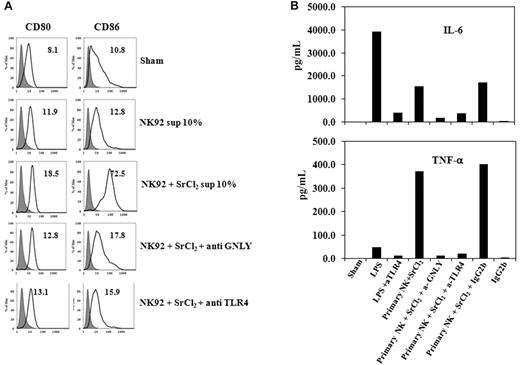
Degranulated NK cells release GNLY to activate bystander APCs
To further assess whether this effect was physiologically relevant, we analyzed whether supernatants of degranulated NK cells could activate DC and if GNLY was required for this activation. We treated both NK92 cell line and primary NK cells with SrCl2, which within 18-24 hours causes degranulation of cells without causing cellular toxicity.35,36 Supernatants from such SrCl2 degranulated NK92 cell lines as well as primary NK cells effectively activated monocyte-derived DCs leading to phenotypic activation (Figure 7A) and production of proinflammatory cytokines like IL-6 and TNFα (Figure 7B). This activation was partially dependent on GNLY, as the effect was neutralized when the protein was depleted by immunoprecipitation. To further confirm whether TLR4 was involved in GNLY-mediated activation, we used blocking antibodies against TLR4 before treating DCs with GNLY containing supernatants. As seen in Figure 7, GNLY required TLR4 to mature or activate DCs, as blocking the receptor abrogated the effect of GNLY present in the supernatants.
Granulysin released from NK cells upon degranulation activates DCs. Mo-iDCs were cultured at 1 × 106 cells/mL in the presence or absence of concentrated supernatants (10% of final volume) from SrCl2-treated NK92 (A) or primary NK cells (B) for 48 hours. Ultrapure LPS (1 μg/mL) was used a positive control. Cells were then analyzed for expression of costimulatory molecules on Mo-DCs by FACS (A) and production of cytokines by Mo-DC (B). For panel A, shaded gray area represents isotype control. Data are shown as geometric mean fluorescence of intensity. One representative experiment of 2 is shown.
Granulysin released from NK cells upon degranulation activates DCs. Mo-iDCs were cultured at 1 × 106 cells/mL in the presence or absence of concentrated supernatants (10% of final volume) from SrCl2-treated NK92 (A) or primary NK cells (B) for 48 hours. Ultrapure LPS (1 μg/mL) was used a positive control. Cells were then analyzed for expression of costimulatory molecules on Mo-DCs by FACS (A) and production of cytokines by Mo-DC (B). For panel A, shaded gray area represents isotype control. Data are shown as geometric mean fluorescence of intensity. One representative experiment of 2 is shown.
The fact that activation of DCs by GNLY was mediated by TLR4 in a MyD88-dependent manner raised the issue of endotoxin contamination of the GNLY preparations. Both the recombinant 9-kDa (produced in E coli) and 15-kDa (produced in mammalian cells) forms of GNLY preparations tested negative by the Limulus Amebocyte Lysate assay, indicating any endotoxin contamination was below the detectable level (< 1 EU/μg protein). In addition, GNLY-induced DC activation was completely blocked by boiling or proteinase K digestion, whereas LPS-induced DC activation was not affected by such treatments. Furthermore, treatment of LPS or GNLY with the mAb DH10 that recognizes both 9- and 15-kDa forms of GNLY completely neutralized the capacity of GNLY to induce DC production of IL-6. On the contrary, LPS-induced IL-6 production was unaffected (supplemental Figure 5). These data collectively demonstrated that the DC-activating activity of GNLY was protein-specific and not due to endotoxin contamination.
Discussion
Certain antimicrobial proteins that exhibit alarmin properties contribute to both innate defense and adaptive immunity by activating multiple receptors on host cells.27-30 These molecules rapidly mobilize the immune system to respond to infection and tissue injury to mediate an immediate inflammatory response that ultimately leads to wound healing and homeostasis. The granules of neutrophils, monocytes, and eosinophils contain several endogenous peptide alarmins, and NK and T cells can now be added to this list. Activated T cells and NK cells release several mediators including cytolytic GNLY, a highly cationic peptide with a broad spectrum of antimicrobial and tumoricidal effects. Several studies have confirmed that the cytolytic activity of the 9-kDa GNLY occurs in the 50-100μM range.37
It has previously been reported that the 9-kDa recombinant human GNLY could induce migration of human peripheral blood monocytes and mature DCs,32 but not Mo-iDCs or murine DCs. We confirmed that 9-kDa GNLY could induce the migration of monocyte-derived mature dendritic cells (data not shown) in vitro. In this study we observed that both 9- and 15-kDa GNLY were also able to induce migration of immature Mo-DC in vitro at nanomolar concentrations. This effect was mediated through a PTx-sensitive GiPCR. The molecular identity of the chemotactic receptor remains unknown and needs further investigation. Although no murine homolog has been identified, injection of GNLY induced a marked recruitment of mouse peritoneal inflammatory cells including neutrophils and CD11b+veGr1+veF4/80+ve monocyte/macrophage-like cells as early as 4 hours followed by a substantial increase in macrophage and CD11c positive DC populations by 24 hours. Because GNLY was also chemotactic in vitro for BMDCs, mice evidently express chemotactic receptors that respond to GNLY. On the other hand, it is likely that recruitment of inflammatory cells in the peritoneal cavity is mediated both by a combination of a direct (receptor-mediated) as well as an indirect (through induction of chemokines) effects. Thus GNLY has the capacity to attract inflammatory cells in response to danger signals.
Activation of monocytes by GNLY led us to believe that it may be a potent mediator of proinflammatory responses. Correspondingly, we observed GNLY to be a potent activator of both Mo-DCs and freshly isolated CD1c-positive DCs as evidenced by (1) enhanced expression of costimulatory molecules, (2) augmented proinflammatory cytokine production, and (3) enabling DCs to acquire the capacity to stimulate proliferation of allogeneic lymphocytes in vitro. Because DCs play a crucial role in regulating both innate and adaptive immune responses, it is likely that high concentrations of GNLY, like other alarmins in the inflammatory environment, may accelerate DC maturation and enable them to become functionally activated and potentiate antigen presentation and trigger antigen-specific immune responses. Although serum concentrations of GNLY under inflammatory conditions have been reported to be at nanomolar levels, higher micromolar levels (100-200 μg/mg tissue) were found in stage II and III gastric cancer tumors.11,13,15-17,38 Hence, it is possible for GNLY to be present at a much higher concentrations in the local inflammatory microenvironment. Degranulating NK cells and CTLs may also deliver relatively high concentrations of GNLY onto the surface of target cells. Consequently, we used pathophysiologically relevant concentrations in our studies.
Though chemotactic mobilization of Mo-DCs was observed at nanomolar concentrations in agreement with previous observations,32 we were unable to detect activation of these cells at a concentration below 2μM for the 9-kDa form, suggesting that both 9-kDa and 15-kDa GNLY interact with different receptors with varied affinity for chemotaxis and activation. It is possible that receptor cross-linking and/or multimerization by the ligand may account for the requirement for high concentration of GNLY for cell activation. On the other hand, the 15-kDa form was 10 times more potent than the posttranscriptionally processed 9-kDa protein, as it was able to induce modest cytokine production by DCs at a concentration as low as 132nM (2 μg/mL). One possible reason for the difference in potency of the 2 forms of the molecule could be attributed to the intrinsic physiologic function of the 2 forms. The 15-kDa form is the precursor of the 9-kDa form. The 9-kDa form is stored in cytotoxic granules, while the 15-kDa form is constitutively secreted. The 9-kDa form is cytotoxic and upon activation is released in granules. The 15-kDa form is constitutively released and is more proinflammatory. Both are chemoattractants and can activate APCs. Nevertheless, the recombinant 9-kDa form has potent antimicrobial activity and is cytolytic on a variety of tumors. The 9-kDa form is in cytotoxic granules, and this compartment is not refilled until the CTLs degranulate. Evidence that the 9-kDa form is derived from posttranslational modification of the 15-kDa form was shown by transfecting the YT cell line with the 15-kDa GNLY cDNA. These cells produce both the 9- and 15-kDa forms, as evidenced by Western blot.21 Therefore, the potent activating effect of the 15-kDa form in our experiments leads us to propose that different forms of GNLY may have distinct roles with the 15-kDa being more proinflammatory.
The finding that human recombinant GNLY could recruit inflammatory cells in a mouse model and activate DCs led us to investigate its potential as an immune adjuvant. Coadministration of human GNLY with OVA to mice not only enhanced humoral responses, but also led to activation of T lymphocytes, inducing both Th1 and (to a lesser extent) Th2 responses, indicating its potential to induce adaptive immune responses and providing the first evidence that GNLY acts as an adjuvant in vivo. This is probably based on its capacity to recruit monocytes and potential APC-like macrophages and DCs, thus enhancing antigen uptake and processing by these sentinel APCs.
Among the various DC-activating stimulants, many TLR ligands activate DCs in a MyD88-dependent manner. Initial reports in literature suggested that TLRs only recognized exogenous pathogen-associated molecular patterns or ligands. However, increasing evidence points toward recognition of endogenous ligands released during tissue injury or inflammation as TLR ligands. Many proteins have been reported to act as endogenous TLR ligands, including heat-shock proteins, hyaluronidase, eosinophil-derived neurotoxin, S100 proteins, mouse β-defensin-2, and HMGB1, which activate APCs through various TLRs.39-41 These findings were confirmed in mouse models and indicated that the TLRs are also involved in sensing endogenous signals, and these effects may be independent of exogenous pathogenic signals recognized during disease or infections.
Using TLR4 mutant mice, we demonstrated that GNLY-mediated recruitment and activation of APCs was dependent on TLR4. In addition, we also demonstrated that the adjuvant activity of GNLY required TLR4. We excluded endotoxin contamination by showing that the denatured and degraded variants of the protein were inactive and by using neutralizing antibodies against the conformationally active protein (mAb DH10 does not react with denatured proteins on sodium dodecyl sulfate–polyacrylamide gel electrophoresis). To further confirm pathophysiologic relevance, we performed experiments showing that granulysin released in supernatants from degranulated NK cell line NK92 or freshly isolated primary NK cells activated Mo-DCs. This effect was partially mediated by GNLY and was blocked by anti-GNLY antibodies and anti-TLR4 antibodies in vitro. Thus it was evident that apart from other inducible factors like cytokines or danger-associated molecular patterns, activated NK cells or T cells release sufficient amount of GNLY by degranulation to activate bystander myeloid cells. Consequently, our data also confirms that the proinflammatory effect was mediated by the protein rather than any endotoxin contaminant and identified GNLY as another endogenous ligand for TLR4.
It is clear that GNLY acts as another endogenous danger signal in inflammatory conditions and is capable of recruiting and activating APCs and enhancing antigen-specific immune responses by using TLR4. The molecular basis for the TLR4-dependent activation of APCs by GNLY requires further studies.
Thus, of the various alarmins identified to date, GNLY is the only NK cell– and T cell–derived peptide to be identified as an alarmin and to potentially play an important role in mobilizing both innate and adaptive immune responses.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Drs O. M. Zack Howard, Stefanie Vogel, and Stephen K. Anderson for their critical suggestions and discussion.
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organization imply endorsement by the US Government. This project has been funded in whole or in part with federal funds from the NCI, National Institutes of Health, under contract N01-CO-12400. The publisher or recipient acknowledges right of the US Government to retain a nonexclusive, royalty-free license in and to any copyright covering the article.
National Institutes of Health
Authorship
Contribution: P.T., G.d.l.R., and Y.L. performed experiments; M.W.F. expressed and purified the recombinant Granulysin; P.T., D.Y., A.M.K., C.C., and J.J.O. contributed to experimental design and data analysis; P.T. and J.J.O. compiled the manuscript; and D.Y., A.M.K., C.C., and J.J.O. revised the manuscript.
Conflict-of-interest disclosure: A.M.K. and C.C. hold patents on granulysin. The remaining authors declare no competing financial interests.
Correspondence: Poonam Tewary, LMI, CIP, CCR, NCI-Frederick, 1050 Boyles St, PO Box B, Rm 31-19, Bldg 560, Frederick, MD 21702; e-mail: tewaryp@mail.nih.gov; or Joost J. Oppenheim, LMI, CIP, CCR, NCI-Frederick, 1050 Boyles St, PO Box B, Rm 21-89A, Bldg 560, Frederick, MD 21702; e-mail: oppenhej@mail.nih.gov.

![Figure 6. Granulysin-mediated cognate immune responses are hampered in TLR4 mutant mice. C3H/HeN and HeJ mice (4 mice per group) were injected intraperitoneally either with 50 μg of OVA alone or with 15-kDa GNLY (20 μg/mouse) or alum. One week later, mice were boosted with the same combination. After 2 days, mice were killed, and the ability to induce OVA-specific splenocyte proliferation (A) and cytokine production (B) was measured. Splenocytes from individual spleens from each group (5 × 105/0.2 mL/well) were stimulated with 50 μg/mL OVA for 72 hours with [3H]-TdR pulse (0.5 μCi/well) for the last 18 hours. For cytokine measurement, (1 × 106/0.2 mL/well) cells from individual spleen were plated with 50 μg/mL OVA, and supernatants were collected after 72 hours. Splenocyte proliferation (mean ± SD) [3H]-TdR incorporation (counts per minute) of triplicate wells and cytokine production from individual mice of 1 experiment representative of 2 are shown. *P < .01, **P < .001, ***P < .0005. ns, not significant.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/116/18/10.1182_blood-2010-03-273953/4/m_zh89991059400006.jpeg?Expires=1769087395&Signature=eEC9H9DOB9If2lAKKJwGYf-OfG4wlBp4MrZ8Mx577abFwv7lNErUi6o5THcSm5lBN5A64n8jW29nGQzcaEo14GSiCnYscjdw4B5s8HmPOhS09JmoMUE-Y~lYOh~jAUcGbcPfsm5vXVQGyyxlw7brJe8z7L~Prxy-BmoT5xqIe2n-XxwUUlAP8CXSXYHbSuFsabys0ftgXQNweHLSaL3qy~Nfkz8xqvrQoceWShVG31z3zZj~D9bZZqliOvVBXtzcar5PmvIkvbivzj9Xx~KvfPdsTF9lVvwvZ~el7C91JdGdT7m9zhzQ-AA~oQtP5x25CVkuKl4I2vZWV8uAIXv86w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal