In this issue of Blood, Berentsen and coworkers1 describe a high response rate which is durable in some patients who receive combination fludarabine and rituximab for chronic cold agglutinin disease (CAD). If confirmed, this is a significant advance in therapy for a frequently difficult clinical problem.
Cold agglutinins (CA) are autoantibodies to red cell carbohydrate antigens that are found in low titer in healthy adults. The majority are IgM proteins.2,3 CA are not cryoglobulins. Monoclonal CA were described in the 1950s in patients with chronic immune hemolytic anemia and thus were the first M-proteins shown to have antibody activity. Christenson and Dacie demonstrated then that many patients with high-titer CA have or subsequently develop serum M-spikes that can be removed by absorption in the cold with red cells bearing the I or i antigen.4 Monoclonal CA often have high thermal amplitude that contributes to their pathogenicity in causing complement-dependent hemolysis (see figure). Many CA bind to red cells at temperatures near 37°C and then fix complement. Because of red cell agglutination at room temperature, clumping may be seen grossly in the tube and automated blood counts are misleading. Blood smears also show red cell clumping. At 37°C, the IgM antibody comes off the cell but complement (C3) remains. Thus the direct antiglobulin test is of the “non-gamma” type (negative with anti-IgG). The monoclonal CA in chronic CAD differ from the lower titer polyclonal IgM CA associated with Mycoplasma pneumonia and viral infections that occasionally cause transient hemolytic anemia. Patients with CA commonly have acrocyanosis, Raynaud phenomenon, or hematuria after cold exposure. Some patients with chronic CAD have IgM monoclonal gammopathy of undetermined significance (MGUS), but others have Waldenström macroglobulinemia (WM). Individuals with chronic CAD often present earlier than other WM patients.5,6 Because of the cold sensitivity and hemolysis, chronic CAD is included in the “IgM-related” classification of WM.7 The VH4-34 gene segment is required to encode anti I and i specificities and these antibodies share cross idiotypic specificity.3,5,6 Some are mutated; others are not. The same gene sequence has been found to encode bacterial anti-lipopolysaccharide (LPS) reactivity as well as other autospecificities, supporting the possibility that B cells containing this VH gene segment may be an integral part of the innate immune system.
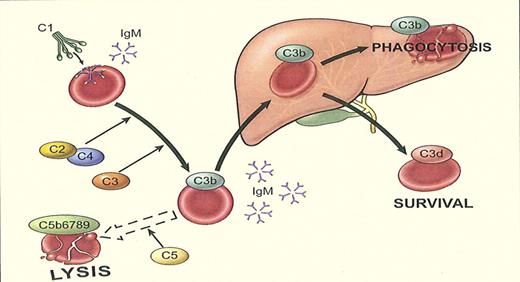
Cooling of the blood during passage through peripheral vessels allows immunoglobulin M (IgM) cold agglutinin to bind to erythrocytes, causing agglutination and complement protein 1 (C1) fixation. C1 esterase activates C4 and C2, generating C3 convertase, which binds and splits C3, leading to deposition of C3b on the cell surface. During return to the central circulation and subsequent warming, IgM removes into serum and the agglutinated cells are detached from each other. C3b remains bound and could activate C5, leading to the formation of the membrane attack complex and intravascular hemolysis, which seems to play a role during acute exacerbations. In steady state, however, phagocytosis of C3b-coated erythrocytes by reticulo-endothelial cells in the liver is the predominant pathway, resulting in extravascular hemolysis. Intrahepatic C3b conversion leads to deposition of C3d on the surviving erythrocytes, which are released into circulation.8 (Image from Clinical Lymphoma & Myeloma, reprinted with permission.)
Cooling of the blood during passage through peripheral vessels allows immunoglobulin M (IgM) cold agglutinin to bind to erythrocytes, causing agglutination and complement protein 1 (C1) fixation. C1 esterase activates C4 and C2, generating C3 convertase, which binds and splits C3, leading to deposition of C3b on the cell surface. During return to the central circulation and subsequent warming, IgM removes into serum and the agglutinated cells are detached from each other. C3b remains bound and could activate C5, leading to the formation of the membrane attack complex and intravascular hemolysis, which seems to play a role during acute exacerbations. In steady state, however, phagocytosis of C3b-coated erythrocytes by reticulo-endothelial cells in the liver is the predominant pathway, resulting in extravascular hemolysis. Intrahepatic C3b conversion leads to deposition of C3d on the surviving erythrocytes, which are released into circulation.8 (Image from Clinical Lymphoma & Myeloma, reprinted with permission.)
Regardless of the pathway by which they develop, monoclonal CA clearly bind red cell autoantigens and cause disease. The obvious first step in treatment of patients with CA is avoiding cold but this is only variably successful. Conventional therapy that produces responses in warm antibody immune hemolytic anemia, viz corticosteroids and/or splenectomy, is largely ineffective in chronic CAD. Thus, the report from Berentsen et al in this issue constitutes a clear step forward. This same group previously reported an increased response rate in CAD patients treated with the monoclonal anti-CD20 antibody, rituximab.8 In the present study, they added a purine nucleoside analog, fludarabine, which has activity in many non-Hodgkin lymphomas including WM. Both agents reduce clonal lymphoproliferation and the production of pathogenic monoclonal IgM. In the Norwegian multicenter study, 29 chronic CAD patients were treated intermittently with rituximab and oral fludarabine over a 3-month period. Twenty-one patients had histologic evidence of a clonal bone marrow disorder (12 with lymphoplasmacytic lymphoma, 6 with marginal zone lymphoma, and 3 unclassified). Twenty-two patients (76%) responded, with 6 (21%) achieving complete remission and 16 (55%) partial remission. Seven patients previously unresponsive to rituximab monotherapy had remission with rituximab plus fludarabine. The estimated median response duration was more than 66 months. Adverse effects were associated with this regimen, however. Grade 3 or 4 hematologic toxicity occurred in 12 patients (41%). Hematologic toxicity may be higher than with the same regimen in other lymphomas. Three patients also had reactivation of herpes zoster.
This study is important for at least 2 reasons. First, complete responses have seldom, if ever, been documented in chronic CAD. Second, the estimated duration of response is more than 5 years.
What is the next step? Because of the hematologic toxicity, lower doses and a modified schedule of fludarabine administration should be explored. In addition, this nucleoside analog is known to be associated with warm antibody immune hemolytic anemia in some CLL patients. Although not seen in the Norwegian study, this possibility remains worrisome. Long-term T-cell immunosuppression is another concern with fludarabine. For these reasons, future investigators should examine reduced doses of fludarabine in combination with rituximab when treating chronic CAD patients.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal