Abstract
The long-term prognosis of indolent adult T-cell leukemia-lymphoma (ATL) is not clearly elucidated. From 1974 to 2003, newly diagnosed indolent ATL in 90 patients (65 chronic type and 25 smoldering type) was analyzed. The median survival time was 4.1 years; 12 patients remained alive for more than 10 years, 44 progressed to acute ATL, and 63 patients died. The estimated 5-, 10-, and 15-year survival rates were 47.2%, 25.4%, and 14.1%, respectively, with no plateau in the survival curve. Although most patients were treated with watchful waiting, 12 patients were treated with chemotherapy. Kaplan-Meier analyses showed that advanced performance status (PS), neutrophilia, high concentration of lactate dehydrogenase, more than 3 extranodal lesions, more than 4 total involved lesions, and receiving chemotherapy were unfavorable prognostic factors for survival. Multivariate Cox analysis showed that advanced PS was a borderline significant independent factor in poor survival (hazard ratio, 2.1, 95% confidence interval, 1.0-4.6; P = .06), but it was not a factor when analysis was limited to patients who had not received chemotherapy. The prognosis of indolent ATL in this study was poorer than expected. These findings suggest that even patients with indolent ATL should be carefully observed in clinical practice. Further studies are required to develop treatments for indolent ATL.
Introduction
Adult T-cell leukemia-lymphoma (ATL) is a peripheral T-lymphocytic malignancy associated with human T-cell lymphotropic virus type 1 (HTLV-1).1 ATL has been classified into 4 clinical subtypes: acute, lymphoma, chronic, and smoldering.2 In general, acute and lymphoma types of ATL have a extremely poor prognosis despite advances in chemotherapy and allogenic hematopoietic stem cell transplantation3-5 because of multidrug resistance, a large tumor burden with multiorgan failure, hypercalcemia, and/or frequent infectious complications associated with a T-cell immunodeficiency. A previous study, in which Japanese patients with ATL were followed for a maximum duration of 7 years, reported that the 4-year survival rates for acute, lymphoma, chronic, and smoldering type were 5.0%, 5.7%, 26.9%, and 62.8%, respectively, with the median survival time (MST) of 6.2 months, 10.2 months, 24.3 months, and not yet reached, respectively.2 Therefore, the chronic and smoldering subtypes of ATL are considered indolent and are usually managed with watchful waiting until disease progression to acute crisis, similar to the management of chronic lymphoid leukemia or smoldering myeloma. However, the follow-up duration of the previous Japanese study was too short for indolent ATL to evaluate the overall risk of progression to acute or lymphoma types (ie, aggressive ATL). A recent Brazilian study, in which patients with ATL were followed for a maximum duration of 14 years, reported that the MST of chronic and smoldering types were 18 months and 58 months, respectively, and the overall survival (OS) rates were less than 20% in both types.6 Their results suggest that the long-term prognosis of indolent ATL might be worse than expected.
The long-term prognosis of Japanese patients with indolent ATL has not been well evaluated so far. Prognostic factors for patients with indolent ATL are also unclear. In the present study, we investigated the long-term outcome of 90 patients with indolent ATL. The purposes of this study were to estimate the 5-, 10-, and 15-year survival rates for indolent ATL and to evaluate the prognostic factors.
Methods
Patients
We evaluated a total of 90 patients with indolent ATL (25 smoldering type and 65 chronic type) who were newly diagnosed at the Nagasaki University Hospital between July 1974 and December 2003. The distribution of patients by year of diagnosis in decades (1974-1983, 1984-1993, and 1994-2003) are presented in Table 1. The cutoff date for analysis was December 2008. The diagnosis of ATL was based on clinical features, histologically and/or cytologically proven mature T-cell malignancy, the presence of anti–HTLV-1 antibody, and monoclonal integration of HTLV-1 proviral DNA into tumor cells as described previously.2,7-9 The subtypes of ATL were classified according to criteria established by the Lymphoma Study Group of Japan Clinical Oncology Group.2 Clinical data included date of diagnosis, complications at diagnosis, therapy regimens if applicable, date of death, cause of death, and date of latest contact. This retrospective, nonrandomized, observational study that used existing data was granted an exemption from the institutional review board and waived the requirement for written informed consent.
Distribution of patients in 3 decades from 1974 to 2003
| Year . | Total no. of patients . | No. of smoldering type (% of total) . | No. of chronic type (% of total) . |
|---|---|---|---|
| 1974-1983 | 19 | 2 (10.5) | 17 (89.5) |
| 1984-1993 | 35 | 7 (20.0) | 28 (80.0) |
| 1994-2003 | 36 | 16 (44.4) | 20 (55.6) |
| Total for all years | 90 | 25 (27.8) | 65 (72.2) |
| Year . | Total no. of patients . | No. of smoldering type (% of total) . | No. of chronic type (% of total) . |
|---|---|---|---|
| 1974-1983 | 19 | 2 (10.5) | 17 (89.5) |
| 1984-1993 | 35 | 7 (20.0) | 28 (80.0) |
| 1994-2003 | 36 | 16 (44.4) | 20 (55.6) |
| Total for all years | 90 | 25 (27.8) | 65 (72.2) |
Clinical factors and definitions
Age was dichotomized into 2 groups: 60 years or older and younger than 60 years. Performance status (PS) was based on the 5-grade scale of the World Health Organization. Complications at diagnosis were dichotomized into present and absent. Leukocytosis was defined as white blood cell count of 12 × 109/L or greater with the median value as cutoff level. Lymphocytosis was defined as a total lymphocyte count of 6.5 × 109/L or greater with the median value as cutoff level. Neutrophilia was defined as a neutrophil count of 7.5 × 109/L or greater.10 Eosinophilia was defined as an eosinophil count of 0.4 × 109/L greater.11 Lactate dehydrogenase (LDH) and blood urea nitrogen (BUN) were dichotomized into normal and elevated concentrations.12 Albumin was dichotomized into concentrations of 40.0 g/L (4.0 g/dL) or greater and less than 40.0 g/L (4.0 g/dL).2 Potential prognostic factors (PPFs) for chronic ATL were defined as those with at least one of the following 3 factors: low serum albumin, high LDH, or high BUN according to previous reports.13,14 Tumor lesions were evaluated as the number of lymph node lesions, number of extranodal lesions, and number of total involved lesions. Extranodal lesions were defined as follows: bone marrow (BM) involvement as the presence of more than 5% typical ATL cells on a BM smear or detection of their infiltration in a BM biopsy specimen; skin involvement as the presence of ATL infiltration in a skin biopsy specimen or as the clinically presence of typical types of skin lesions such as tumors, nodules, erythema, and papules, if biopsy was impossible; lung involvement as lesions with ATL cell infiltration in a transbronchial lung biopsy specimen or in bronchoalveolar lavage fluid; liver involvement as hepatomegaly determined by any imaging tests or liver biopsy if done; spleen involvement as splenomegaly on any imaging test. All patients had peripheral blood involvement. Both lymph node and extranodal tumor lesions were determined according to Ann Arbor classification.2 The number of total involved lesions was defined as the sum of lymph node lesions and extranodal lesions.2 Factors used in analyses were listed in Table 2.
Statistical analysis
OS was defined as the time from the date of first diagnosis to the date of death or the latest contact with the patient. Survival curves were estimated using the Kaplan-Meier method and were compared using the generalized Wilcoxon test. MST was estimated as the time point at which the Kaplan-Meier survival curves crossed 50%. Time to transformation was calculated as the time from the date of the first diagnosis to the date of transformation into the aggressive type (acute or lymphoma type). Univariate and multivariate Cox regression analyses were applied to evaluate prognostic factors for survival. The effects of clinical parameters were evaluated as hazard ratios (HRs) and their 95% confidence intervals (95% CIs). All statistical analyses were performed using SAS software (Version 9.1; SAS Japan Institute). All tests were 2-tailed, and the statistical significance level was set at .05.
Results
Baseline characteristics
The median value of white blood cell count, lymphocyte count, neutrophil count, and eosinophil count was 11.5 × 109/L (range, 3.9-94.4 × 109/L), 6.5 × 109/L (range, 0.9-80.2 × 109/L), 4.9 × 109/L (range, 1.5-25.5 × 109/L), and 0.06 × 109/L (range, 0-3.0 × 109/L), respectively. Frequencies of the patients at baseline are summarized in Table 2. Fifty-eight percent of the patients were male, 52% were 60 years or older, and 22% had an advanced PS (2 or more grade). Regarding complications, 35 patients (39%) had some complications at the time of diagnosis, including 13 with chronic pulmonary diseases (10 chronic bronchitis, 2 diffuse panbronchiolitis, and 1 bronchial asthma with chronic bronchitis), 9 with opportunistic infections (3 pneumocystis pneumonia, 2 cryptococcal meningitis, 2 aspergillus pneumonia, 1 cytomegalovirus infection, and 1 pulmonary tuberculosis), 7 with malignancies other than ATL (2 lung cancer, 1 larynx cancer, 1 pharynx cancer, 1 colon cancer, 1 hepatic cell carcinoma, and 1 lip cancer), and 6 with autoimmune diseases (2 infective dermatitis, 1 primary biliary cirrhosis, 1 autoimmune hemolytic anemia, 1 dermatomyositis, and 1 ulcerative colitis). The 6 patients with autoimmune diseases had received a variety of medications as follows: antibiotics for infective dermatitis, ursodeoxycholic acid for primary biliary cirrhosis, prednisolone for autoimmune hemolytic anemia and dermatomyositis, and sulfasalazine for ulcerative colitis. Concerning the hematologic factors, 43 patients (48%) had leukocytosis, 45 (50%) had lymphocytosis, 17 (19%) had neutrophilia, and 17 (19%) had eosinophilia. Regarding the laboratory factors, 28 patients (31%) had a high LDH level (greater than the normal limit). Only 5 of 87 patients (6%) had an abnormal BUN level; 34 of 88 patients (39%) had a low albumin level. Forty-seven patients (55%) had more than 1 of the 3 unfavorable prognostic factors.
Survival by baseline clinical factors
| Factors . | No. of evaluated (% of total) . | No. of deaths (%)* . | MST, y . | Cumulative probability of survival† . | ||
|---|---|---|---|---|---|---|
| 5-y survival, % (95% CI) . | 10-y survival, % (95% CI) . | P† . | ||||
| Total | 90 | 63 (70) | 4.1 | 47.2 (36.1-57.5) | 25.4 (15.3-36.8) | |
| Clinical subtype | ||||||
| Smoldering | 25 (28) | 17 (68) | 2.9 | 39.4 (19.8-58.6) | 25.3 (8.2-47.0) | .36 |
| Chronic | 65 (72) | 46 (71) | 5.3 | 50.2 (37.0-62.0) | 26.3 (14.6-39.5) | |
| Patient-related factors (n = 90) | ||||||
| Sex | ||||||
| Male | 52 (58) | 34 (65) | 4.3 | 48.1 (33.4-61.3) | 24.9 (11.8-40.5) | .99 |
| Female | 38 (42) | 29 (76) | 4.1 | 46.4 (29.5-61.6) | 26.5 (12.0-43.4) | |
| Age | ||||||
| 60 y or older | 46 (52) | 32 (70) | 3.7 | 45.5 (30.4-59.4) | 29.5 (14.8-45.8) | .18 |
| Younger than 60 y | 44 (48) | 31 (70) | 4.5 | 49.2 (32.9-63.6) | 24.0 (11.2-39.3) | |
| PS | ||||||
| 0 | 22 (24) | 15 (68) | 8.4 | 75.9 (51.4-89.1) | 38.9 (16.8-60.7) | .006 |
| 1 | 49 (54) | 33 (67) | 3.4 | 41.5 (26.9-55.5) | 22.5 (9.7-38.5) | |
| 2 or 3 | 19 (22) | 15 (79) | 1.3 | 27.9 (10.2-49.0) | 13.9 (1.3-41.1) | |
| Complications at diagnosis (n = 90) | ||||||
| Absent | 55 (61) | 37 (67) | 5.7 | 54.1 (39.4-66.7) | 25.4 (12.9-40.1) | |
| Present | 35 (39) | 26 (74) | 3.4 | 36.6 (20.7-52.8) | 28.3 (13.5-45.1) | .06 |
| Malignancies other than ATL | 7 (8) | 6 (86) | 0.8 | 28.6 (4.1-61.2) | 28.6 (4.1-61.2) | |
| Opportunistic infection | 9 (10) | 7 (78) | 1.2 | 0 | 0 | |
| Chronic pulmonary disease | 13 (14) | 10 (77) | 4.1 | 38.5 (14.1-62.8) | 25.6 (5.2-53.4) | |
| Autoimmune disease | 6 (7) | 3 (50) | 11.4 | 62.5 (14.2-89.3) | 62.5 (14.2-89.3) | |
| Hematologic factors | ||||||
| WBC count (n = 90) | ||||||
| At least 12.0 × 109/L | 43 (48) | 32 (74) | 3.4 | 43.0 (27.6-57.5) | 22.3 (9.9-37.8) | .24 |
| Less than 12.0 × 109/L | 47 (52) | 31 (66) | 5.3 | 51.0 (35.1-64.8) | 28.5 (13.6-45.2) | |
| Total lymphocyte count (n = 90) | ||||||
| At least 6.5 × 109/L | 45 (50) | 35 (78) | 3.7 | 43.3 (28.2-57.5) | 17.4 (6.8-32.0) | .34 |
| Less than 6.5 × 109/L | 45 (50) | 28 (62) | 5.3 | 51.4 (35.2-65.4) | 36.8 (20.9-52.9) | |
| Neutrophil counts (n = 89) | ||||||
| At least 7.5 × 109/L | 17 (19) | 14 (82) | 2.3 | 29.4 (10.7-51.1) | 14.7 (1.3-42.9) | .05 |
| Less than 7.5 × 109/L | 72 (81) | 48 (67) | 5.3 | 51.0 (38.3-62.4) | 28.4 (16.6-41.3) | |
| Eosinophil count (n = 89) | ||||||
| At least 0.4 × 109/L | 17 (19) | 11 (65) | 4.0 | 34.9 (13.0-58.0) | 23.2 (4.9-49.4) | .47 |
| Less than 0.4 × 109/L | 72 (81) | 51 (71) | 4.5 | 49.2 (36.8-60.5) | 27.4 (16.0-40.1) | |
| Laboratory factors | ||||||
| LDH (n = 90) | ||||||
| Greater than NI | 28 (31) | 23 (82) | 1.5 | 34.8 (17.3-53.0) | 14.9 (3.9-32.7) | .004 |
| Less than or equal to NI | 62 (69) | 40 (65) | 5.4 | 52.9 (39.2-64.8) | 31.8 (18.5-45.9) | |
| BUN (n = 87) | ||||||
| Greater than NI | 5 (6) | 5 (100) | 2.0 | 20.0 (0.8-58.2) | 0 | .18 |
| Less than or equal to NI | 82 (94) | 56 (68) | 4.5 | 48.9 (37.2-59.6) | 28.4 (17.3-40.6) | |
| Albumin (n = 88) | ||||||
| Less than 40.0 g/L | 34 (39) | 22 (65) | 3.4 | 39.9 (22.4-56.8) | 25.6 (8.9-46.4) | .22 |
| At least 40.0 g/L | 54 (61) | 40 (74) | 5.3 | 52.2 (37.9-64.7) | 26.6 (14.3-40.6) | |
| Potential prognostic factors (n = 87)‡ | ||||||
| At least 1 | 47 (55) | 34 (72) | 2.9 | 38.7 (24.1-53.1) | 18.1 (6.5-34.3) | .05 |
| None | 40 (45) | 27 (68) | 5.4 | 56.1 (39.2-70.0) | 35.2 (19.3-51.6) | |
| Tumor lesions (n = 90) | ||||||
| No. of lymph node lesions | ||||||
| 2 or more | 24 (27) | 16 (67) | 2.1 | 37.5 (19.0-56.0) | 30.0 (12.1-50.4) | .09 |
| 0 or 1 | 66 (73) | 47 (71) | 5.3 | 50.9 (37.5-62.8) | 23.6 (12.2-37.2) | |
| No. of extranodal lesions | ||||||
| 3 or more | 18 (20) | 14 (78) | 1.1 | 29.4 (10.7-51.1) | 19.6 (4.2-43.3) | .005 |
| 1 or 2 | 72 (80) | 49 (68) | 5.3 | 51.6 (38.9-62.9) | 26.8 (15.2-39.7) | |
| No. of total involved lesions | ||||||
| 4 or more | 24 (27) | 16 (67) | 1.3 | 34.8 (16.6-53.7) | 26.1 (8.8-47.6) | .03 |
| 2 or 3 | 42 (46) | 30 (71) | 4.5 | 49.5 (32.7-64.3) | 13.1 (3.5-29.1) | |
| 1 | 24 (27) | 17 (71) | 5.4 | 54.5 (32.1-72.4) | 44.1 (22.8-63.5) | |
| Chemotherapy | ||||||
| Received | 12 (13) | 12 (100) | 1.4 | 25.0 (6.0-50.5) | 0 | .01 |
| Not received | 78 (87) | 51 (65) | 5.3 | 50.8 (38.6-61.8) | 31.3 (19.3-44.0) | |
| Factors . | No. of evaluated (% of total) . | No. of deaths (%)* . | MST, y . | Cumulative probability of survival† . | ||
|---|---|---|---|---|---|---|
| 5-y survival, % (95% CI) . | 10-y survival, % (95% CI) . | P† . | ||||
| Total | 90 | 63 (70) | 4.1 | 47.2 (36.1-57.5) | 25.4 (15.3-36.8) | |
| Clinical subtype | ||||||
| Smoldering | 25 (28) | 17 (68) | 2.9 | 39.4 (19.8-58.6) | 25.3 (8.2-47.0) | .36 |
| Chronic | 65 (72) | 46 (71) | 5.3 | 50.2 (37.0-62.0) | 26.3 (14.6-39.5) | |
| Patient-related factors (n = 90) | ||||||
| Sex | ||||||
| Male | 52 (58) | 34 (65) | 4.3 | 48.1 (33.4-61.3) | 24.9 (11.8-40.5) | .99 |
| Female | 38 (42) | 29 (76) | 4.1 | 46.4 (29.5-61.6) | 26.5 (12.0-43.4) | |
| Age | ||||||
| 60 y or older | 46 (52) | 32 (70) | 3.7 | 45.5 (30.4-59.4) | 29.5 (14.8-45.8) | .18 |
| Younger than 60 y | 44 (48) | 31 (70) | 4.5 | 49.2 (32.9-63.6) | 24.0 (11.2-39.3) | |
| PS | ||||||
| 0 | 22 (24) | 15 (68) | 8.4 | 75.9 (51.4-89.1) | 38.9 (16.8-60.7) | .006 |
| 1 | 49 (54) | 33 (67) | 3.4 | 41.5 (26.9-55.5) | 22.5 (9.7-38.5) | |
| 2 or 3 | 19 (22) | 15 (79) | 1.3 | 27.9 (10.2-49.0) | 13.9 (1.3-41.1) | |
| Complications at diagnosis (n = 90) | ||||||
| Absent | 55 (61) | 37 (67) | 5.7 | 54.1 (39.4-66.7) | 25.4 (12.9-40.1) | |
| Present | 35 (39) | 26 (74) | 3.4 | 36.6 (20.7-52.8) | 28.3 (13.5-45.1) | .06 |
| Malignancies other than ATL | 7 (8) | 6 (86) | 0.8 | 28.6 (4.1-61.2) | 28.6 (4.1-61.2) | |
| Opportunistic infection | 9 (10) | 7 (78) | 1.2 | 0 | 0 | |
| Chronic pulmonary disease | 13 (14) | 10 (77) | 4.1 | 38.5 (14.1-62.8) | 25.6 (5.2-53.4) | |
| Autoimmune disease | 6 (7) | 3 (50) | 11.4 | 62.5 (14.2-89.3) | 62.5 (14.2-89.3) | |
| Hematologic factors | ||||||
| WBC count (n = 90) | ||||||
| At least 12.0 × 109/L | 43 (48) | 32 (74) | 3.4 | 43.0 (27.6-57.5) | 22.3 (9.9-37.8) | .24 |
| Less than 12.0 × 109/L | 47 (52) | 31 (66) | 5.3 | 51.0 (35.1-64.8) | 28.5 (13.6-45.2) | |
| Total lymphocyte count (n = 90) | ||||||
| At least 6.5 × 109/L | 45 (50) | 35 (78) | 3.7 | 43.3 (28.2-57.5) | 17.4 (6.8-32.0) | .34 |
| Less than 6.5 × 109/L | 45 (50) | 28 (62) | 5.3 | 51.4 (35.2-65.4) | 36.8 (20.9-52.9) | |
| Neutrophil counts (n = 89) | ||||||
| At least 7.5 × 109/L | 17 (19) | 14 (82) | 2.3 | 29.4 (10.7-51.1) | 14.7 (1.3-42.9) | .05 |
| Less than 7.5 × 109/L | 72 (81) | 48 (67) | 5.3 | 51.0 (38.3-62.4) | 28.4 (16.6-41.3) | |
| Eosinophil count (n = 89) | ||||||
| At least 0.4 × 109/L | 17 (19) | 11 (65) | 4.0 | 34.9 (13.0-58.0) | 23.2 (4.9-49.4) | .47 |
| Less than 0.4 × 109/L | 72 (81) | 51 (71) | 4.5 | 49.2 (36.8-60.5) | 27.4 (16.0-40.1) | |
| Laboratory factors | ||||||
| LDH (n = 90) | ||||||
| Greater than NI | 28 (31) | 23 (82) | 1.5 | 34.8 (17.3-53.0) | 14.9 (3.9-32.7) | .004 |
| Less than or equal to NI | 62 (69) | 40 (65) | 5.4 | 52.9 (39.2-64.8) | 31.8 (18.5-45.9) | |
| BUN (n = 87) | ||||||
| Greater than NI | 5 (6) | 5 (100) | 2.0 | 20.0 (0.8-58.2) | 0 | .18 |
| Less than or equal to NI | 82 (94) | 56 (68) | 4.5 | 48.9 (37.2-59.6) | 28.4 (17.3-40.6) | |
| Albumin (n = 88) | ||||||
| Less than 40.0 g/L | 34 (39) | 22 (65) | 3.4 | 39.9 (22.4-56.8) | 25.6 (8.9-46.4) | .22 |
| At least 40.0 g/L | 54 (61) | 40 (74) | 5.3 | 52.2 (37.9-64.7) | 26.6 (14.3-40.6) | |
| Potential prognostic factors (n = 87)‡ | ||||||
| At least 1 | 47 (55) | 34 (72) | 2.9 | 38.7 (24.1-53.1) | 18.1 (6.5-34.3) | .05 |
| None | 40 (45) | 27 (68) | 5.4 | 56.1 (39.2-70.0) | 35.2 (19.3-51.6) | |
| Tumor lesions (n = 90) | ||||||
| No. of lymph node lesions | ||||||
| 2 or more | 24 (27) | 16 (67) | 2.1 | 37.5 (19.0-56.0) | 30.0 (12.1-50.4) | .09 |
| 0 or 1 | 66 (73) | 47 (71) | 5.3 | 50.9 (37.5-62.8) | 23.6 (12.2-37.2) | |
| No. of extranodal lesions | ||||||
| 3 or more | 18 (20) | 14 (78) | 1.1 | 29.4 (10.7-51.1) | 19.6 (4.2-43.3) | .005 |
| 1 or 2 | 72 (80) | 49 (68) | 5.3 | 51.6 (38.9-62.9) | 26.8 (15.2-39.7) | |
| No. of total involved lesions | ||||||
| 4 or more | 24 (27) | 16 (67) | 1.3 | 34.8 (16.6-53.7) | 26.1 (8.8-47.6) | .03 |
| 2 or 3 | 42 (46) | 30 (71) | 4.5 | 49.5 (32.7-64.3) | 13.1 (3.5-29.1) | |
| 1 | 24 (27) | 17 (71) | 5.4 | 54.5 (32.1-72.4) | 44.1 (22.8-63.5) | |
| Chemotherapy | ||||||
| Received | 12 (13) | 12 (100) | 1.4 | 25.0 (6.0-50.5) | 0 | .01 |
| Not received | 78 (87) | 51 (65) | 5.3 | 50.8 (38.6-61.8) | 31.3 (19.3-44.0) | |
WBC indocates white blood cell count; MST, median survival time (years); and NI, normal index.
Rate of death in evaluated cases.
Cumulative probability of survival rate was estimated with the Kaplan-Meier method, and the P value was calculated with the generalized Wilcoxon test.
Twenty-four patients (27%) had more than 2 involved lymph node lesions. Regarding the extranodal lesions, skin involvement was observed in 46 patients (51%), liver involvement in 15 (17%), spleen involvement in 6 (7%), and pulmonary involvement in 1 (1%). Of the 64 patients who had BM examined, the involvement was observed in 16 patients (25%; data not shown). Twenty percent of the patients (n = 18) had more than 3 extranodal lesions. Regarding the number of total involved lesions (extranodal lesions plus lymph node lesions), more than 4 involved lesions were observed in 24 patients (27%), 2 or 3 involved lesions in 42 patients (46%), and only 1 involved lesion in 24 patients (27%).
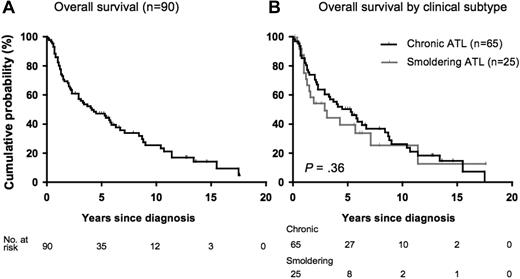
Prognosis
Among 90 patients with indolent ATL, 63 (70%) died, with a median duration of follow-up of 4.1 years (range, 8 days to 17.6 years). The estimated 5-, 10-, and 15-year survival rates were 47.2% (95% CI, 36.1%-57.5%), 25.4% (95% CI, 15.3%-36.8%), and 14.1% (95% CI, 6.2%-25.3%), respectively, with an MST of 4.1 years (95% CI, 2.9-6.3 years; Figure 1A). No plateaus were observed in the survival curves for OS. Of the 27 survivors, 12 were alive for more than 10 years. Of the 63 patients who died, 41 (65.1%) died of acute ATL after transformation, 5 (7.9%) died of severe chronic ATL, 11 (17.5%) died of other diseases (3 malignancies other than ATL, 2 chronic pulmonary diseases, 2 opportunistic infections, 2 autoimmune diseases, 1 cardiac failure, and 1 myocardial infarction), 2 died of transplantation-related complications, and 4 died of unknown cause. No significant difference in OS was observed between patients who died of ATL and patients who died of other causes (data not shown). Among 90 patients, 44 (49%) progressed to aggressive ATL (all were acute types), among those, 41 (93%) died. The median time to transformation was 18.8 months (range, 0.3 months to 17.6 years).
Survival of patients with indolent ATL. (A) For OS (n = 90), the median survival time was 4.1 years (95% CI, 2.9-6.3 years). No plateau was observed in the survival curves for OS. The estimated 5-, 10-, and 15-year survival rates were 47.2% (95% CI, 36.1%-57.5%), 25.4% (95% CI, 15.3%-36.8%), and 14.1% (95% CI, 6.2%-25.3%), respectively. (B) OS by clinical subtype (smoldering type vs chronic type). The estimated 15-year survival rate was 12.7% (95% CI, 1.1%-38.8%) with an MST of 2.9 years for smoldering type and 14.7% (95% CI, 5.7%-27.8%) with an MST of 5.3 years. There was no statistically significant difference (P = .36).
Survival of patients with indolent ATL. (A) For OS (n = 90), the median survival time was 4.1 years (95% CI, 2.9-6.3 years). No plateau was observed in the survival curves for OS. The estimated 5-, 10-, and 15-year survival rates were 47.2% (95% CI, 36.1%-57.5%), 25.4% (95% CI, 15.3%-36.8%), and 14.1% (95% CI, 6.2%-25.3%), respectively. (B) OS by clinical subtype (smoldering type vs chronic type). The estimated 15-year survival rate was 12.7% (95% CI, 1.1%-38.8%) with an MST of 2.9 years for smoldering type and 14.7% (95% CI, 5.7%-27.8%) with an MST of 5.3 years. There was no statistically significant difference (P = .36).
Among 25 patients with smoldering ATL, 17 patients (68%) died, and the estimated 15-year survival rate was 12.7% (95% CI, 1.1%-38.8%) with an MST of 2.9 years (95% CI, 1.3-7.1 years). Of the 17 patients who died, 15 died of acute ATL after transformation. Among 65 patients with chronic ATL, 46 (71%) died, and the estimated 15-year survival rate was 14.7% (95% CI, 5.7%-27.8%) with an MST of 5.3 years (95% CI, 2.9-6.7 years). Of the 46 patients who died, 29 died of acute ATL after transformation and 5 died of the disease severity. No statistically significant difference was observed in OS between subtypes (P = .36; Figure 1B). The overall estimated 5- and 10-year survival rates of both subtypes are shown in Table 2.
Effects of clinical factors on prognosis
Effects of clinical factors on prognosis were analyzed with the use of all the 90 patients together. Results of prognostic analyses (estimated 5- and 10-year OS rates and MST) with the use of Kaplan-Meier methods are summarized in Table 2. The survival rate was poor for patients with advanced PS (P = .006; Figure 2A), neutrophilia (P = .05; Figure 2B), and a higher LDH level (P = .004; Figure 2C). Patients with at least 1 of 3 PPFs for chronic ATL (a high level of LDH and BUN and a low level of albumin)13,14 showed a poor survival rate compared with patients without (P = .05; Figure 2D). The difference in survival rates between patients with any complications and patients without was marginally significant (P = .06). Among patients with any complications, those with malignancies other than ATL or opportunistic infections at diagnosis showed a tendency of poor prognosis, although the number of patients in each category was too small (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). Although no difference was observed in survival rates between patients with involvement of more than 2 lymph node lesions and patients with less involvement (P = .09; Table 2), the survival rate of patients with more than 3 extranodal lesions was significantly poor than the others (P = .005; Figure 2E). The survival rate was worse in patients with more than 4 total involvement lesions than in the others (Table 2). Of the extranodal lesions, we additionally examined the effect of skin lesion and BM involvement on survival rates. The survival rate of patients with BM involvement was significantly poor than of patients without (P = .04; data not shown), but that of patients with skin involvement was not different from those without (P = .66; supplemental Figure 2).
OS by clinical parameters. (A) OS by PS (P = .006). (B) OS by neutrophil count (P = .05). The unit is ×109/L. (C) OS by LDH level (P = .004). NI indicates normal index. (D) OS by PPFs for chronic ATL that were defined based on low serum albumin, high LDH, or high BUN according to previous reports13,14 (P = .05). (E) OS by the number of extranodal lesions (EXNL; P = .005). (F) OS by treatment states (P = .01).
OS by clinical parameters. (A) OS by PS (P = .006). (B) OS by neutrophil count (P = .05). The unit is ×109/L. (C) OS by LDH level (P = .004). NI indicates normal index. (D) OS by PPFs for chronic ATL that were defined based on low serum albumin, high LDH, or high BUN according to previous reports13,14 (P = .05). (E) OS by the number of extranodal lesions (EXNL; P = .005). (F) OS by treatment states (P = .01).
Although most patients in this study had not been treated until their disease progression was similar to B-cell chronic lymphoid leukemia, 12 patients with chronic ATL were treated with chemotherapy immediately after diagnosis because of elevated LDH levels in 8 patients, severe BM involvement in 2 patients, and severe skin involvements in 2 patients. Among them, 2 patients were treated with VCAP (vincristine, cyclophosphamide, doxorubicin, and prednisone)–AMP (doxorubicin, ranimustine, and prednisone)–VECP (vindesine, etoposide, carboplatin, and prednisone),3 2 with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), 4 with CHOP-like, 3 with VEPA (vincristine, etoposide, prednisone, and doxorubicin),15 and 1 with low-dose etoposide. All of these patients died (MST, 1.4 years; 95% CI, 1.1-2.3 years), and their prognosis was very poor compared with patients not treated (P = .01; Figure 2F).
On the basis of results from Kaplan-Meier curves and univariate analysis for each factor, we decided to include PS category, dichotomized neutrophil counts, dichotomized LDH category, dichotomized number of extranodal lesions, the number of total involved lesions, and chemotherapy states into multivariate Cox analysis. Model A included PS category, dichotomized neutrophil counts, dichotomized LDH category, dichotomized number of extranodal lesions, and chemotherapy states. Model B included the same factors as model A except for the number of total involved lesions instead of the number of extranodal lesions. This was because, by definition, a factor of the number of total involved lesions included a factor of the number of extranodal lesions. Results were summarized in Table 3. In model A, advanced PS (≥ 2; HR, 2.1; 95% CI, 1.0-4.6; P = .06, borderline significance) and chemotherapy states (HR, 2.3; 95% CI, 1.1-4.7; P = .03, significance) were correlated with OS, but the remaining factors were not independent prognostic factors after adjustment for covariate factors. To evaluate effects of clinical factors beyond the effect of chemotherapy states on OS, we also performed additional multivariate analyses for patients who were not received chemotherapy (n = 78; model C and model D in Table 3). We found that there was no clinical parameter that associated with OS.
Effects of clinical factors on OS in Cox analyses
| Clinical factor . | All patients (n = 90) . | Patients had not received chemotherapy (n = 78) . | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate analysis . | Multivariate model A . | Multivariate model B . | Univariate analysis . | Multivariate model C . | Multivariate model D . | |||||||
| HR (95% CI) . | P . | HR (95% CI) . | P . | HR (95% CI) . | P . | HR (95% CI) . | P . | HR (95% CI) . | P . | HR (95% CI) . | P . | |
| PS | ||||||||||||
| 0 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 1 | 1.5 (0.8-2.7) | .22 | 1.4 (0.8-2.8) | .27 | 1.3 (0.7-2.6) | .37 | 1.4 (0.7-2.7) | .28 | 1.6 (0.8-3.1) | .21 | 1.4 (0.7-2.9) | .30 |
| 2 or more | 2.5 (1.2-5.2) | .01 | 2.1 (1.0-4.6) | .06 | 2.1 (1.0-4.6) | .06 | 1.7 (0.7-4.0) | .26 | 1.5 (0.6-3.8) | .39 | 1.6 (0.6-4.2) | .30 |
| Neutrophil counts | ||||||||||||
| Less than 7.5 × 109/L | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 7.5 × 109/L or greater | 1.6 (0.9-2.9) | .15 | 1.3 (0.6-2.7) | .45 | 1.2 (0.6-2.3) | .58 | 1.3 (0.6-2.7) | .47 | 1.5 (0.6-3.8) | .43 | 1.0 (0.5-2.3) | .94 |
| LDH | ||||||||||||
| Less than or equal to NI | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Greater than NI | 1.7 (1.0-2.9) | .04 | 1.5 (0.8-2.7) | .16 | 1.5 (0.8-2.6) | .21 | 1.5 (0.8-2.8) | .19 | 1.7 (0.9-3.3) | .12 | 1.6 (0.8-3.1) | .20 |
| No. of extranodal lesions | ||||||||||||
| 0-2 | 1 | 1 | 1 | 1 | ||||||||
| 3 or more | 1.5 (0.8-2.8) | .16 | 0.7 (0.3-1.6) | .41 | 0.9 (0.4-2.2) | .82 | 0.5 (0.1-1.6) | .22 | ||||
| No. of total involved lesions | ||||||||||||
| 1 | 1 | 1 | 1 | 1 | ||||||||
| 2 or 3 | 1.2 (0.7-2.2) | .52 | 0.8 (0.4-1.6) | .52 | 1.1 (0.6-2.1) | .67 | 0.9 (0.4-1.7) | .65 | ||||
| 4 or more | 1.5 (0.7-3.0) | .26 | 0.9 (0.4-2.1) | .83 | 1.0 (0.5-2.3) | .96 | 0.8 (0.3-2.0) | .67 | ||||
| Chemotherapy | ||||||||||||
| Not received | 1 | 1 | 1 | |||||||||
| Received | 2.6 (1.4-5.1) | .003 | 2.3 (1.1-4.7) | .03 | 2.0 (1.0-4.2) | .06 | ||||||
| Clinical factor . | All patients (n = 90) . | Patients had not received chemotherapy (n = 78) . | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate analysis . | Multivariate model A . | Multivariate model B . | Univariate analysis . | Multivariate model C . | Multivariate model D . | |||||||
| HR (95% CI) . | P . | HR (95% CI) . | P . | HR (95% CI) . | P . | HR (95% CI) . | P . | HR (95% CI) . | P . | HR (95% CI) . | P . | |
| PS | ||||||||||||
| 0 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 1 | 1.5 (0.8-2.7) | .22 | 1.4 (0.8-2.8) | .27 | 1.3 (0.7-2.6) | .37 | 1.4 (0.7-2.7) | .28 | 1.6 (0.8-3.1) | .21 | 1.4 (0.7-2.9) | .30 |
| 2 or more | 2.5 (1.2-5.2) | .01 | 2.1 (1.0-4.6) | .06 | 2.1 (1.0-4.6) | .06 | 1.7 (0.7-4.0) | .26 | 1.5 (0.6-3.8) | .39 | 1.6 (0.6-4.2) | .30 |
| Neutrophil counts | ||||||||||||
| Less than 7.5 × 109/L | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 7.5 × 109/L or greater | 1.6 (0.9-2.9) | .15 | 1.3 (0.6-2.7) | .45 | 1.2 (0.6-2.3) | .58 | 1.3 (0.6-2.7) | .47 | 1.5 (0.6-3.8) | .43 | 1.0 (0.5-2.3) | .94 |
| LDH | ||||||||||||
| Less than or equal to NI | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Greater than NI | 1.7 (1.0-2.9) | .04 | 1.5 (0.8-2.7) | .16 | 1.5 (0.8-2.6) | .21 | 1.5 (0.8-2.8) | .19 | 1.7 (0.9-3.3) | .12 | 1.6 (0.8-3.1) | .20 |
| No. of extranodal lesions | ||||||||||||
| 0-2 | 1 | 1 | 1 | 1 | ||||||||
| 3 or more | 1.5 (0.8-2.8) | .16 | 0.7 (0.3-1.6) | .41 | 0.9 (0.4-2.2) | .82 | 0.5 (0.1-1.6) | .22 | ||||
| No. of total involved lesions | ||||||||||||
| 1 | 1 | 1 | 1 | 1 | ||||||||
| 2 or 3 | 1.2 (0.7-2.2) | .52 | 0.8 (0.4-1.6) | .52 | 1.1 (0.6-2.1) | .67 | 0.9 (0.4-1.7) | .65 | ||||
| 4 or more | 1.5 (0.7-3.0) | .26 | 0.9 (0.4-2.1) | .83 | 1.0 (0.5-2.3) | .96 | 0.8 (0.3-2.0) | .67 | ||||
| Chemotherapy | ||||||||||||
| Not received | 1 | 1 | 1 | |||||||||
| Received | 2.6 (1.4-5.1) | .003 | 2.3 (1.1-4.7) | .03 | 2.0 (1.0-4.2) | .06 | ||||||
HR indicates hazard ratio; 95% CI, 95% confidence interval; and NI, normal index.
Discussion
In the present study, we investigated for the first time the long-term clinical course of patients with indolent ATL with a maximum duration of follow-up of 17.6 years. We found that the prognosis of indolent ATL was poor with the MST of 4.1 years, and the estimated 15-year OS rates were 14.1% with no plateau in the survival curve. The prognosis observed in the present study was poorer than expected. Our results confirmed a recent long-term Brazilian study,6 that showed a poor OS of less than 20% for indolent ATL. In the present study, we showed that 65.1% of patients died of acute ATL with a median time to transformation of 18.8 months. This finding suggests that most patients with indolent ATL will eventually die of aggressive ATL during their long-term course of illness. These findings suggest that even patients with indolent ATL should be carefully observed by frequent clinical visits.
The cause of death in patients with indolent ATL has not been well reported so far. In the present study, patients with indolent ATL died of various causes such as malignancies other than ATL, chronic pulmonary diseases, opportunistic infections, and autoimmune diseases, in addition to death from acute ATL after transformation. A previous long-term study, which followed-up 50 HTLV-1 carriers with monoclonal proliferation of T lymphocytes (pre-ATL) for 20 years, also reported that 10 patients died of opportunistic infections such as Pneumocystis pneumonia or malignancies other than ATL (skin carcinoma, lung cancer, etc).16 Patients with indolent ATL were also comorbid with a variety of diseases at diagnosis such as chronic pulmonary disease, opportunistic infections, multiple cancers, and autoimmune diseases in the present study. The pathogens responsible for the opportunistic infections were similar to those observed in patients with AIDS associated with HIV. Opportunistic infection was previously reported as a frequent complication in patients with aggressive or with indolent ATL.2 These findings suggest that helper T-cell function in indolent ATL might be impaired similar to that in AIDS.17
We also presented that chronic pulmonary disease, multiple cancers, and autoimmune diseases were frequent as complications at diagnosis in indolent ATL. The reason why indolent ATL had such immune dysregulation remains unknown. It was recently noted that the origin of the ATL cells in a fraction of the patients was from regulatory T cells expressing FoxP3 and CCR4.18,19 In the present study, 6 patients also had autoimmune diseases. Among them, 3 patients were treated with immunosuppressive drugs, and of those only one patient with smoldering ATL transformed to acute ATL. Therefore, we were not able to evaluate the effect of comorbid autoimmune diseases and immunosuppressive drug therapy on the risk of transformation or poor prognosis so far. Further studies are warranted to elucidate the mechanisms responsible for the development of hyperimmunity or hypoimmunity in patients with indolent ATL.
Although comparison on OS by subtype is not a primary purpose of this study, it was unexpected that survival rates of smoldering ATL (15-year OS, 12.7%) tended to be lower than chronic ATL (15-year OS, 14.7%), and the MST of smoldering ATL (2.9 years) tended to be shorter than chronic ATL (5.3 years; Table 2; Figure 1B). Transformation rates of smoldering ATL and chronic ATL were 60% (n = 15) and 44% (n = 29), respectively (data not shown), which was also unexpected. Although there was no statistically difference in OS, MST, and transformation rate between the 2 groups, our results were different from a previous short-time follow-up study reported by Shimoyama et al2 (the 4-year survival rates for smoldering type was 62.8%). It was unknown why the rate of smoldering type was poorer than chronic type in the present study. Some previous studies suggested that skin involvements might be a risk factor for poor prognosis of smoldering ATL.6,20-22 In the present study, the frequency of patients with skin lesion was a little higher in smoldering ATL (n = 14; 56%) than in chronic ATL (n = 32; 49%). The OS of smoldering ATL with skin lesion was worse than that of chronic ATL without skin lesion (supplemental Figure 2), although there was no statistical difference (P = .5). Therefore, a possible explanation might be that smoldering ATL with poor conditions (eg, skin involvement) might be disproportionately included in the present study because data were collected at a university hospital, where more advanced cases were referred from city clinics. Another possible explanation might be that the percentage of patients with smoldering-type ATL has increased recently, as shown in Table 1. In recent decades, more patients have been diagnosed with the smoldering type of ATL on the basis of a health examination, including a blood cell count. Some of these patients may have been in the early phase of acute ATL.
Shimoyama et al2 reported that involved lymph node lesions, extranodal lesions, and total involvement lesions were significantly poor prognostic factors for ATL all together, and low serum albumin, high LDH, or high BUN levels were PPFs for chronic ATL.13,14 As we expected, patients with at least 1 of 3 known PPFs for chronic ATL (a high level of LDH and BUN and a low level of albumin)13,14 showed a poor survival rate than patients without (Table 2; Figure 2D). We also confirmed the difference was seen when analyses were performed for chronic ATL only (P = .03) but was not seen for smoldering ATL only (P = .62; supplemental Figure 3). This suggests that there may be different prognostic factors for smoldering ATL and chronic ATL, respectively. Further detailed studies regarding prognostic factors are needed for individual subtype.
Other than the known 3 potential prognostic factors, an advanced PS, neutrophilia, more than 3 extranodal lesions, more than 4 total involved lesions, and having received chemotherapy were shown to be possible unfavorable prognostic factors for indolent ATL in our Kaplan-Meier analyses (Table 2; Figures 1B, 2A-F). However, in multivariate Cox analyses, only advanced PS and chemotherapy state were associated with OS after adjustment for other covariates (models A and B in Table 3). The poor prognosis in patients with indolent ATL who were treated by chemotherapy was similar to that of the patients with unfavorable chronic ATL who were treated with intensive combination chemotherapy in several clinical trials in Japan.3,5,23 Although advanced PS was a borderline significant independent poor factor on survival for indolent ATL in the model that used all patients, the factor was not a prognostic factor anymore when data were limited for only untreated patients (models C and D in Table 3). Among 12 patients who received chemotherapy, 7 (58%) had advanced PS at diagnosis. This suggests that patients with advanced PS at diagnosis might have a condition that required treatments, which introduced the disappearance of the effect of advanced PS on survival, even though advanced PS was an independent poor factor.
Regarding the effect of the presence of extranodal lesions on poor survival, we previously reported that BM involvement was a prognostic factor for aggressive ATL.24 Although we did not present the effect of each extranodal lesion on survival in detail, we also confirmed that the survival rate of patients with BM involvement was significantly poor compared with patients those without BM involvement (P = .04; data not shown), but the survival rate of patients with skin involvement was not different compared with those without (P = .66; supplemental Figure 2). However, some studies reported that the presence of skin lesions was a possible poor prognostic factor in indolent ATL,6,20-22 as described earlier. Setoyama et al21 reported that smoldering cases with a deeper infiltration pattern had a more aggressive course than cases with a superficial infiltration pattern. Degree of skin involvement might be associated with prognosis in indolent ATL.
Previously, our study group noted that some patients showed alterations in tumor suppressor genes (p16 INKA25,26 or p5327 ) or aneuploidy greater than 1 chromosomal locus by comparative genomic hybridization in ATL cells28 and that such abnormalities were associated with a poor prognosis. Although we could not perform molecular analyses for all patients in the present study, 7 were examined molecularly, and at least one abnormality was found in each patient (data not shown). They had a poor prognosis and died within 2.5 years. Patients with a poor prognosis who died during the first steep slope in the survival curve (Figure 1A) might have had such genetic alterations.
The primary purpose of this study was to analyze prognosis of smoldering and chronic types together as an indolent type of ATL. Therefore, we were not able to present in detail the difference in prognostic factors between subtypes, which is one of the limitations in this study. The number of cases evaluated in this study was too small to perform detail analyses for prognostic factors in indolent ATL. Further large-scaled studies are warranted.
In conclusion, the long-term prognosis of patients with indolent ATL was not good without a plateau phase in the survival curve. Further studies are warranted to elucidate patients with indolent ATL who require intensive chemotherapy, allogenic hematopoietic stem cell transplantation (in cases of aggressive ATL), or combination therapy with zidovudine and interferon alfa.29,30 In addition, new molecular targeting treatments, such as histone deacetylase inhibitors,31 which have shown promise in the treatment of CD4+ cutaneous T-cell lymphoma, should be taken into consideration for treatment of indolent ATL.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank the many hematologists in the Department of Hematology and Molecular Medicine, Atomic Bomb Disease Institute, Nagasaki University, Graduate School of Biomedical Sciences, for the diagnosis and treatment of patients with ATL.
No grants or financial support were provided for this study.
Authorship
Contribution: Y.T. collected and analyzed the data and wrote the manuscript; M.I. analyzed the data and wrote the manuscript; Y.I., M.T., T.J., T.K., Y.Y., S.K., S.I., Y.M., and M.T. made the diagnoses and treated the patients with ATL; and K.T. organized the study.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Masako Iwanaga, Department of Molecular Medicine and Hematology, Atomic Bomb Disease Institute, Nagasaki University Graduate School of Biomedical Sciences, 1-12-4 Sakamoto, Nagasaki 852-8523, Japan; e-mail: masakoiwng@gmail.com.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal