Abstract
Studies have reported inconsistent evidence for an association between venous thrombosis and arterial cardiovascular events. We further studied the association between both diseases by comparing the occurrence of cardiovascular events in patients diagnosed with acute pulmonary embolism (PE) contrasted to patients with comparable baseline risk characteristics (patients in whom PE was clinically suspected but ruled out). Included were 259 patients with provoked PE, 95 patients with unprovoked PE, and 334 control patients without PE. Patients diagnosed with PE were treated with vitamin K antagonists for 6 months. Median follow-up was 4.2 years. Sixty-three arterial cardiovascular events were registered (incidence, 5.1/100 patient-years). Adjusted hazard ratio was not different between patients with all-cause PE and control patients (1.39, 95% confidence interval [CI], 0.83-2.3) but increased for patients with unprovoked PE versus both patients with provoked PE and control patients without PE (2.18; 95% CI, 1.1-4.5; and 2.62; 95% CI, 1.4-4.9, respectively). This effect was confirmed after redefining the study start date to the moment the vitamin K antagonists were discontinued. Our study underlines the association between unprovoked venous thrombosis and arterial cardiovascular events; however, risk differences between patients with provoked PE and patients in whom PE was clinically suspected but ruled out could not be demonstrated.
Introduction
Recent epidemiologic studies have shown an association between venous thrombosis (VT), that is, deep vein thrombosis as well as pulmonary embolism (PE), and arterial cardiovascular events.1,2 This association can at least in part be explained by the presence of common risk factors for venous and arterial disease, such as obesity and the metabolic syndrome.3-5 It was previously shown that, compared with population controls, the risk of arterial cardiovascular events after a first deep vein thrombosis or a first acute PE was increased in the first year after the VT as well as in 20 years of follow-up.6 Furthermore, patients with VT of unknown origin (unprovoked VT) are at higher risk of developing arterial cardiovascular events than patients with provoked VT.7-9 However, evidence of the relation between VT and arterial cardiovascular events is inconsistent. Two observational studies could not identify increased risk of overall or unprovoked VT in patients with noninvasively measured subclinical atherosclerosis.10,11 In addition, there are no reports in which the incidence of arterial cardiovascular events in patients with VT has been compared with this incidence in controls without VT, but with similar baseline risk characteristics. This is important because population controls in general have a lower a priori risk for arterial disease than patients with established VT.6
We intended to further study the association between VT and arterial cardiovascular events by defining a control population with a more comparable baseline risk characteristic for cardiovascular disease than population controls. We hypothesized that patients in whom PE was clinically suspected but ruled out would provide such a control group. Accordingly, we assessed the incidence of arterial cardiovascular events in patients diagnosed with a first all-cause PE as well as with provoked PE and unprovoked PE separately, and contrasted them with patients in whom a first suspected PE was ruled out.
Methods
Study design
A cohort study was performed to evaluate the risk of arterial cardiovascular events and the event-free survival in patients with a confirmed first PE compared with a population in which a clinically suspected first PE was ruled out. Study endpoints were arterial cardiovascular events defined as otherwise unexplained death, clinically adjudicated acute myocardial infarction, stroke or transient ischemic attack, claudication, unstable angina, carotid endarterectomy, coronary artery bypass graft, peripheral arterial bypass, or angioplasty.11 Both patients with and without PE were followed from the start dates to January 1, 2008, or the occurrence of 1 of the endpoints, whichever came first. After the study period, we searched the medical charts of the study patients for the occurrence of study endpoints, and we contacted them by mail or phone to complete our data with the latest information on their medical history and clinical condition. If patients could not be reached, we used the last medical report of their treating physician or general practitioner. When a patient with or without PE had died, the pathology report was scrutinized to establish the cause of death. In case autopsy was not performed, the probable cause of death was verified with the treating physician or general practitioner. Otherwise, unexplained death was classified as caused by an arterial cardiovascular event. All endpoints were adjudicated by an independent committee. In addition to information on the endpoints, we also collected information on sex, age at inclusion, risk factors for PE, recurrent VT during the study period, and medical history of cardiovascular events in both patients with and without PE. This study was approved by the institutional review board of Leiden University Medical Center, and all participants provided informed consent in accordance with the Declaration of Helsinki.
Patients with acute PE
All patients with proven PE in our hospital are registered in the hospital administration database. Consecutive adult patients with no medical history of VT, diagnosed with a first PE between January 2001 and July 2004, were included in this study. The diagnosis of PE was based on either a positive CT angiogram or a ventilation perfusion scintigraphy indicating a high probability for PE. Data on risk factors for PE were derived from the discharge status of the patients. Unprovoked PE was defined as PE occurring in the absence of risk factors, that is, active malignancy, immobility more than 3 days or recent long flight, recent surgery or fracture of extremity, pregnancy or peripartum period, hormone replacement therapy, and use of oral contraception. Patients were treated according to hospital policy, initially with therapeutic doses of unfractionated heparin or low molecular weight heparin followed by vitamin K antagonists (VKAs). Because VKA therapy has been shown to reduce the risk for myocardial infarction,12 patients with an additional indication for VKA therapy, in whom these anticoagulants could not be withdrawn after a 6-month treatment period, were excluded from this analysis.
Patients in whom acute PE was suspected but ruled out
The control cohort consisted of patients in whom PE was clinically suspected but ruled out by either an unlikely probability (Wells rule ≤ 4 points13 ) in combination with a normal D-dimer test or a CT scan without signs of PE, followed by a 3-month follow-up period without the occurrence of subsequent symptomatic VT. Consecutive patients without PE were recruited between November 2002 and September 2004 and included in a diagnostic management study.14 Only patients who had presented to our hospital and without a medical history of VT or indication for VKA therapy were included in the present analysis.
Statistical analysis
We assessed the incidence of subsequent arterial cardiovascular events in patients with provoked and unprovoked PE compared with patients in whom PE was ruled out. Because we intended to study the role of PE as risk factor for arterial cardiovascular events by defining patient groups with similar baseline risk characteristics, we performed the same analysis after exclusion of patients who had experienced prior arterial cardiovascular events. In addition, to rule out the initial effect of oral anticoagulation therapy, a third analysis was performed in which the start date was set at the time the oral anticoagulant therapy was discontinued; ie, the treatment duration was 6 months, and no recurrent VT had occurred in the patients with PE, and 6 months after PE was excluded in the control patients. The Kaplan-Meier life-table method was used to estimate the cumulative event rate. Patients with recurrent VT during follow-up or death not associated with any cardiovascular event were censored. A Cox proportional hazard model was used to calculate hazard ratios (HR). After multivariate analysis, these were adjusted for potentially important confounders, including sex, age, malignancy, smoking status, blood pressure or lipid-lowering medication, antiplatelet therapy, hormonal contraception, diabetes, and history of cardiovascular events. SPSS Version 14.02 (SPSS Inc), was used for all analyses.
Results
Patients
In the study period, 379 patients were diagnosed with a first PE of whom 356 patients had no additional indication for VKA therapy. In addition, 364 controls were registered.12 We were not able to collect full study information in 30 patients without PE and 2 patients with PE because they refused cooperation (n = 2), lived abroad (n = 7) were not registered with a general practitioner (n = 12), or we did not succeed in retrieving up-to-date contact specifications (n = 11). The final diagnosis in the 334 patients in whom acute PE was suspected but ruled out was musculoskeletal disease in 37 patients (11%), noninfectious or malignancy-associated pulmonary disease in 43 (13%), gastrointestinal disease in 17 (5.1%), infectious disease in 84 (25%), malignancy related in 47 (14%), cardiovascular disease in 33 (9.9%), and other/unknown in 73 patients (22%). Of the 33 patients with cardiovascular disease, 13 had no prior history of cardiovascular events and were discharged with newly prescribed secondary preventive medication (eg, statins, antiplatelet, or blood pressure–lowering medication). The remaining 20 patients were already treated with these medications.
General characteristics of the total study population (n = 688) are depicted in Table 1. There was a difference in the male-to-female ratio, age, and prevalence of active malignancy between the study groups. The fraction of active smokers, the prevalence of diabetes and the use of blood pressure–lowering, antiplatelet and lipid-lowering medication was not different between the 3 study groups. The median follow-up period of the patient cohort was 1451 days (interquartile range, 337-1867 days) and of the control population 1558 days (interquartile range, 1320-1789 days). The total number of patient years was 1284 for the controls, 817 for the patients with provoked PE, and 349 for the patients with unprovoked PE.
General characteristics of the study population
| . | Control patients (n = 334) . | Patients with provoked PE (n = 259) . | Patients with unprovoked PE (n = 95) . |
|---|---|---|---|
| Sex (female), %* | 211 (63) | 137 (53) | 49 (55) |
| Age, y (mean ± SD)*† | 48 ± 17 | 52 ± 18 | 55 ± 17 |
| History of arterial cardiovascular events, n (%)† | 40 (12) | 38 (15) | 17 (18) |
| Active malignancy, n (%)*† | 46 (14) | 103 (40) | — |
| Diabetes, n (%)† | 17 (5.1) | 12 (4.6) | 6 (6.3) |
| Active smoker, n (%)† | 110 (33) | 78 (30) | 30 (32) |
| Use of blood pressure–lowering medication, n (%)‡ | 107 (32) | 91 (35) | 34 (36) |
| Use of antiplatelet therapy, n (%)‡ | 50 (15) | 37 (14) | 17 (18) |
| Use of lipid-lowering medication, n (%)‡ | 57 (17) | 42 (16) | 18 (19) |
| No. of patient-years in follow-up | 1284 | 817 | 349 |
| . | Control patients (n = 334) . | Patients with provoked PE (n = 259) . | Patients with unprovoked PE (n = 95) . |
|---|---|---|---|
| Sex (female), %* | 211 (63) | 137 (53) | 49 (55) |
| Age, y (mean ± SD)*† | 48 ± 17 | 52 ± 18 | 55 ± 17 |
| History of arterial cardiovascular events, n (%)† | 40 (12) | 38 (15) | 17 (18) |
| Active malignancy, n (%)*† | 46 (14) | 103 (40) | — |
| Diabetes, n (%)† | 17 (5.1) | 12 (4.6) | 6 (6.3) |
| Active smoker, n (%)† | 110 (33) | 78 (30) | 30 (32) |
| Use of blood pressure–lowering medication, n (%)‡ | 107 (32) | 91 (35) | 34 (36) |
| Use of antiplatelet therapy, n (%)‡ | 50 (15) | 37 (14) | 17 (18) |
| Use of lipid-lowering medication, n (%)‡ | 57 (17) | 42 (16) | 18 (19) |
| No. of patient-years in follow-up | 1284 | 817 | 349 |
PE indicates pulmonary embolism; and —, not applicable.
Significantly different.
At time of presentation with clinically suspected acute PE.
After hospital discharge.
Venous events
Thirty-seven patients experienced symptomatic recurrent VT during follow-up. Recurrent VT occurred in 12 patients with unprovoked PE with a total of 55.2 patient-years (incidence, 16 of 100 patient-years), in 17 patients with provoked PE with a total of 68.4 patient-years (8.4 of 100 patient-years), and in 8 patients without PE with a total of 22.7 patient-years (1.8 of 100 patient-years; Table 2). The risk for recurrent VT was increased in patients with unprovoked PE compared with patients with provoked PE and patients without PE (relative risk, 1.92; 95% confidence interval [CI], 0.96-3.9 and 5.27, 95% CI, 2.2-13, respectively), and in patients with provoked PE compared with patients without PE (2.74, 95% CI, 1.2-6.3).
Distribution of arterial cardiovascular events and (recurrent) venous thromboembolic events during the follow-up period
| . | Total population, n (%) . | Control population, n (%) . | Patients with provoked PE, n (%) . | Patients with unprovoked PE, n (%) . | RR patients vs controls . | RR unprovoked PE vs controls . | RR provoked PE vs controls . | RR unprovoked vs provoked PE . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR . | 95% CI . | RR . | 95% CI . | RR . | 95% CI . | RR . | 95% CI . | |||||
| Any arterial cardiovascular event | 63 (5.1) | 26 (4.1) | 17 (3.4) | 20 (13) | 1.34 | 0.83-2.2 | 2.70 | 1.6-4.6 | 0.84 | 0.47-1.5 | 3.21 | 1.8-5.8 |
| Myocardial infarction | 14 (0.89) | 4 (0.31) | 4 (0.40) | 6 (4.2) | 2.35 | 0.93-6.0 | 5.27 | 1.9-14 | 1.29 | 0.42-4.0 | 4.09 | 1.5-11 |
| Stroke | 21 (1.3) | 6 (0.87) | 6 (0.92) | 9 (3.7) | 2.35 | 0.93-6.0 | 5.27 | 1.9-14 | 1.29 | 0.42-4.0 | 4.09 | 1.5-11 |
| Other | 28 (2.9) | 16 (2.9) | 7 (2.1) | 5 (5.0) | 0.71 | 0.34-1.5 | 1.10 | 0.41-2.9 | 0.56 | 0.24-1.4 | 1.95 | 0.63-6.0 |
| (Recurrent) VT | 37 (6.0) | 8 (1.8) | 17 (8.4) | 12 (16) | 3.42 | 1.6-7.4 | 5.27 | 2.2-13 | 2.74 | 1.2-6.3 | 1.92 | 0.96-3.9 |
| . | Total population, n (%) . | Control population, n (%) . | Patients with provoked PE, n (%) . | Patients with unprovoked PE, n (%) . | RR patients vs controls . | RR unprovoked PE vs controls . | RR provoked PE vs controls . | RR unprovoked vs provoked PE . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR . | 95% CI . | RR . | 95% CI . | RR . | 95% CI . | RR . | 95% CI . | |||||
| Any arterial cardiovascular event | 63 (5.1) | 26 (4.1) | 17 (3.4) | 20 (13) | 1.34 | 0.83-2.2 | 2.70 | 1.6-4.6 | 0.84 | 0.47-1.5 | 3.21 | 1.8-5.8 |
| Myocardial infarction | 14 (0.89) | 4 (0.31) | 4 (0.40) | 6 (4.2) | 2.35 | 0.93-6.0 | 5.27 | 1.9-14 | 1.29 | 0.42-4.0 | 4.09 | 1.5-11 |
| Stroke | 21 (1.3) | 6 (0.87) | 6 (0.92) | 9 (3.7) | 2.35 | 0.93-6.0 | 5.27 | 1.9-14 | 1.29 | 0.42-4.0 | 4.09 | 1.5-11 |
| Other | 28 (2.9) | 16 (2.9) | 7 (2.1) | 5 (5.0) | 0.71 | 0.34-1.5 | 1.10 | 0.41-2.9 | 0.56 | 0.24-1.4 | 1.95 | 0.63-6.0 |
| (Recurrent) VT | 37 (6.0) | 8 (1.8) | 17 (8.4) | 12 (16) | 3.42 | 1.6-7.4 | 5.27 | 2.2-13 | 2.74 | 1.2-6.3 | 1.92 | 0.96-3.9 |
PE indicates pulmonary embolism; and RR, relative risk.
Deaths
A total of 176 deaths were recorded during the study period. The most frequent cause of death was malignancy (93 cases, 53% of all deaths). Five patients died as a result of myocardial infarction and 5 as a result of severe stroke.
Arterial cardiovascular events
In total, 63 arterial cardiovascular events occurred with a total of 125 patient-years (incidence, 5.1 of 100 patient-years; Table 2). Patients with unprovoked PE had a higher incidence of arterial cardiovascular events (20 events in 44.7 patient-years; 13 of 100 patient-years) than the patients with provoked PE (17 arterial cardiovascular events in 28.1 patient-years; 3.4 of 100 patient-years) and control patients without PE (26 events in 52.6 patient-years; 4.1 of 100 patient-years). In addition, risks for the occurrence of any arterial cardiovascular event as well as for myocardial infarction and for stroke were increased in the patients with unprovoked PE compared with the patients with provoked PE and patients without PE (Table 2). Only slight, nonsignificant differences in the incidence of arterial cardiovascular events were found between overall PE patients and controls.
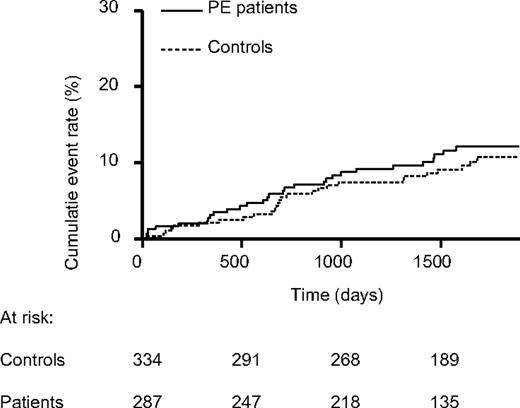
Kaplan-Meier analysis showed no differences between the event-free survival of all PE patients compared with control patients without PE (Figure 1). Corrected for prior arterial events, sex, age, active malignancy, and use of oral anticonceptive medication, HR of all patients with PE was only marginally increased compared with the control patients without PE (1.39; 95% CI, 0.83-2.3).
Cumulative arterial cardiovascular event rate in pulmonary embolism (PE) patients and control patients without PE.
Cumulative arterial cardiovascular event rate in pulmonary embolism (PE) patients and control patients without PE.
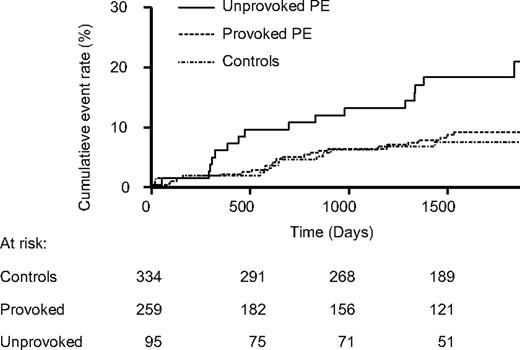
When PE patients were categorized in provoked and unprovoked PE, clear differences emerged in the arterial cardiovascular event-free survival between patients with unprovoked PE and both the patients with provoked PE and without PE (Figure 2). The event-free survival was not much different between patients with provoked PE and control patients without PE. Adjusted HR of patients with unprovoked PE was increased compared with patients with provoked PE (2.18; 95% CI, 1.1-4.5) and control patients without PE (2.62; 95% CI, 1.4-4.9).
Cumulative arterial cardiovascular event rate in patients with unprovoked pulmonary embolism (PE), with provoked PE, and in control patients without PE.
Cumulative arterial cardiovascular event rate in patients with unprovoked pulmonary embolism (PE), with provoked PE, and in control patients without PE.
Prior arterial cardiovascular events were found to be an important predictor for the reoccurrence of arterial cardiovascular events in the follow-up period (odds ratio = 3.10; 95% CI 1.8-5.3). When all study patients with and without PE with a history of arterial cardiovascular events (n = 95) were excluded from the analysis, adjusted hazards of patients with unprovoked PE was increased versus both patients with provoked PE (2.73; 95% CI, 1.1-7.0) and control patients without PE (3.72; 95% CI, 1.6-8.4). No differences were detected between the patients with provoked PE and the control patients without PE.
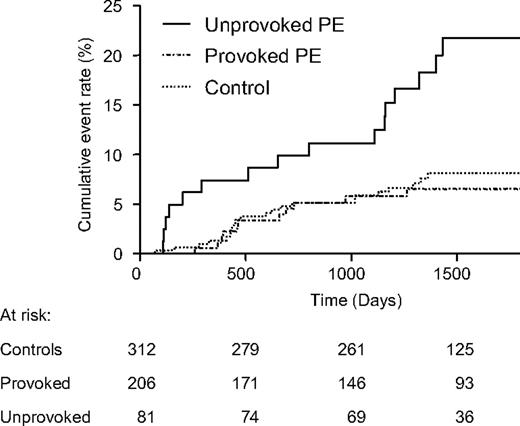
The corrected HR of the third analysis 6 months after initial presentation and after discontinuation of anticoagulant therapy was not different between all patients with PE and the control patients without PE (1.31; 95% CI, 0.74-2.3). In contrast, the cumulative arterial cardiovascular event rate in patients with unprovoked PE was higher than this cumulative event rate in patients with provoked PE (HR = 3.24; 95% CI, 1.4-7.7) and control patients without PE (HR 2.85; 95% CI, 1.4-5.6, Figure 3).
Cumulative arterial cardiovascular event rate in patients with unprovoked pulmonary embolism (PE), with provoked PE, and in control patients without PE starting after a 6-month treatment period for acute PE or 6 months after the exclusion of acute PE.
Cumulative arterial cardiovascular event rate in patients with unprovoked pulmonary embolism (PE), with provoked PE, and in control patients without PE starting after a 6-month treatment period for acute PE or 6 months after the exclusion of acute PE.
Discussion
Our data demonstrate that the incidence of arterial cardiovascular events for all patients with PE was not increased compared with the control patients without PE. However, patients diagnosed with a first unprovoked PE were at higher risk of developing subsequent arterial cardiovascular vascular events than patients with a first provoked PE and our control population without PE. In addition, this event-free survival disadvantage was still demonstrated after exclusion of all PE and control patients with prior arterial cardiovascular events and after redefining the study start date to the moment the VKA treatment was discontinued in the patients initially diagnosed with acute PE.
Our study design was different from previous reports on selection of control patients, start date, and definition of endpoints. Because our study was designed to compare the incidence of arterial cardiovascular events in PE patients and control patients without PE but with comparable risk characteristics, the results firmly establish the earlier described increased occurrence of arterial cardiovascular events after unprovoked VT.7-9 In addition, we performed an additional analysis to rule out the possible confounding effect of VKA and censored all patients who developed VT during the study period. Our finding that control patients without PE and patients with provoked PE have the same arterial cardiovascular event-free survival supports the hypothesis that a shared but yet unidentified mechanism causes events in both venous and arterial systems. Suggested attributive factors are shared risk factors or etiologic pathways as thrombogenesis, endothelial damage, or inflammation.2 Unfortunately, our dataset does not allow us to determine whether unprovoked PE and (early) arterial cardiovascular events are each caused separately by a shared pathway or the occurrence of (early) arterial cardiovascular events after venous thrombosis is related more causally. Future studies should further investigate the pathogenesis behind the observed associations.
Strengths of our study include the long-term follow-up of a large and unselected, consecutive patient cohort. Second, we have used a very comparable control population of patients with clinically suspected but ruled out PE.12 Third, we used clear definitions for our inclusion criteria and endpoints. The latter are serious medical events that are probably recorded accurately.
Limitations of this study are the lost-to-follow-up rate of 4.4% and the relatively limited number of patients in the unprovoked PE cohort. In addition, although we aimed at including a control group for patients with acute PE with similar baseline risk characteristics for cardiovascular disease, several relevant demographics, such as age, sex, medical history, and use of medication, were different between the patients with and the patients without PE. Nonetheless, HRs proved to be significantly elevated for patients with unprovoked PE after adjusting for these factors. Furthermore, because contrast echocardiography was not routinely assessed after the diagnosis of PE, we could not evaluate the possibility of paradoxical embolism as the cause of subsequent arterial events in some patients. Finally, although a predefined diagnostic algorithm for patients with suspected acute PE has been used in all patients, we could not fully correct for possible differences in sensitivity of the diagnostic tests or changes in diagnostic algorithms for our endpoints over time.
In conclusion, this study demonstrates that patients with a first unprovoked PE are at higher risk of developing arterial cardiovascular events than patients with a first provoked PE and specific control patients in whom PE was clinically suspected but ruled out. These results justify large studies to study the underlying pathophysiologic mechanisms that cause the increased risk of arterial cardiovascular events after PE and to identify specific patients at very high risk. These latter patients might benefit from modified treatment regimens to prevent the occurrence of arterial cardiovascular disease, including preventive use of antiplatelet and cholesterol synthesis inhibiting treatment.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: F.A.K. was responsible for study concept and design; acquired, analyzed, and interpreted the data, and drafted the manuscript; I.C.M.M. and L.B. acquired, analyzed, and interpreted the data, and drafted the manuscript; J.T.T. critically revised the manuscript for important intellectual content; F.R.R. analyzed and interpreted the data and critically revised the manuscript for important intellectual content; A.d.R. critically revised the manuscript for important intellectual content; and M.V.H. was responsible for study concept and design, analyzed and interpreted the data, and critically revised the manuscript for important intellectual content.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Frederikus A. Klok, Leiden University Medical Center (C4-70), Albinusdreef 2, Postbus 9600, 2300 RC Leiden, The Netherlands; e-mail: F.A.Klok@LUMC.nl.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal