Abstract
Abstract 987
Poster Board I-9
Port-a-catheters are commonly used as vascular access device in children with Acute Lymphoblastic Leukemia (ALL) requiring long-term chemotherapy. Literature suggests that surgical procedures should not be performed in patients with very low neutrophil counts. Neutropenia, however, is very common in patients with ALL putting them at increased risk for infection and impaired wound healing.
1) To determine if severe neutropenia, defined as neutrophil count < 500/mm3, on the day of port-a-catheter insertion is a risk factor for catheter-associated infection in children with ALL; 2) To evaluate the incidence of catheter-associated infection and wound dehiscence; 3) To assess other potential risk factors for infection, such as ALL risk category, dexamethasone use during induction therapy and nutritional status at the time of port-a-catheter insertion.
This was a retrospective study conducted in children newly diagnosed with ALL (January 2005 to August 2008) who had a port-a-catheter inserted to assess catheter-associated infections and dehiscence. Demographic data, clinical characteristics, port-a-catheter insertion data and complications post-procedure were reviewed. The post-procedure complications were classified as early (≤ 30 days) or late (> 30 days). The end of catheter follow-up was March, 2009. The nutritional status was evaluated using albumin and total protein levels as well as the BMI-for-age z-score or weight-for-age z-score. Statistical analysis included descriptive and inferential statistics (Chi-squared test, Wilcoxon rank sum test and Kaplan-Meier survival curve).
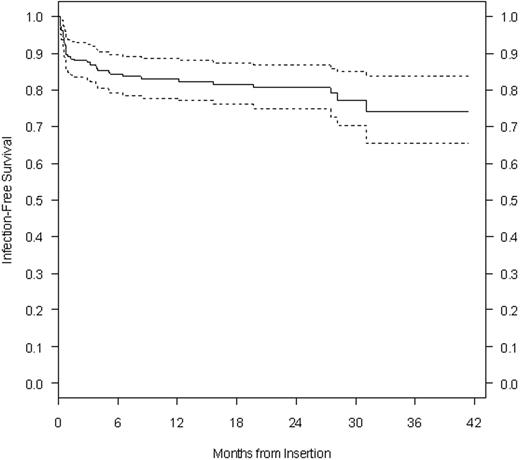
192 port-a-catheters were inserted in 179 patients with ALL in this 3.5 year time period. Most patients were started on chemotherapy 3 days prior to catheter insertion. A total of 43 catheter-associated infections (22.39%) were diagnosed and the infection rate was 0.35/1000 catheter-days. Children with severe neutropenia on the day of insertion (n=99) had a catheter-associated infection rate of 15.15%; whereas, non-severe neutropenic (≥ 500 cells/mm3) children (n=93) had a rate of 24.73%. This difference was not statistically significant (p=0.137). Out of 192 port-a-catheters, 12 (6.25%) had to be removed due to infection. The most common organisms to cause catheter removal were Coagulase Negative Staphylococcus and Staphylococcus aureus. Patients with high risk precursor B and T cell ALL had a statistically significant higher incidence of late catheter-associated infections (p=0.024) than standard risk ALL. Gender (p=0.863), use of dexamethasone during induction (p=0.201), low BMI-for-age z-score or weight-for-age z-score (p=0.659), low albumin (p=0.530), low total protein (p=0.759) and fever pre-procedure (p=0.339) were not risk factors for infection. Patients who had an early catheter-associated infection did not have a greater chance of having a late infection (p=0.813). Out of 9 wound dehiscences (4.68%), 5 presented also with a local infection. The catheter infection-free survival rate at 1 year was 88.6%, at 2 years was 86.7% and at 3 years was 83.9% (see Graph).
This study shows that severe neutropenia on the day of port-a-catheter insertion does not increase the incidence of catheter-associated infection in children with ALL. In contrast, high risk ALL (precursor B and T cell) is a risk factor for late catheter-associated infections.
Graph: Port-a-catheter infection-free rate expressed in months (mean ± 2 standard errors).
Graph: Port-a-catheter infection-free rate expressed in months (mean ± 2 standard errors).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal