Abstract
Abstract 534
Light chain (AL) amyloidosis is characterized by deposition of amyloid derived from immunoglobulin light chains in various organs. Cardiac involvement can lead to a variety of manifestations including congestive heart failure (CHF), conduction disturbances, and arrhythmias, including sudden death. Patients (pts) with cardiac involvement, especially in the presence of CHF, have a poor prognosis. Autologous peripheral blood stem cell transplantation (SCT) is increasingly being used for AL and has been associated with high rates of hematologic and organ responses. However, cardiac involvement due to AL is also associated with higher rates of complications following SCT; and those with advanced cardiac involvement are rarely considered for SCT. As such, our study does not represent the full spectrum of pts with cardiac involvement due to AL, but only those who are considered transplant eligible.
Of the 382 pts with AL who underwent SCT at our institution between May 1996 and September 2008, 194 had documented cardiac involvement. Six pts who underwent heart transplantation were excluded; and188 (49%) pts were considered for this study. Groups were compared using Fisher's exact test or t-test, and survival was calculated using Kaplan Meier method. Survival curves were compared using log rank test.
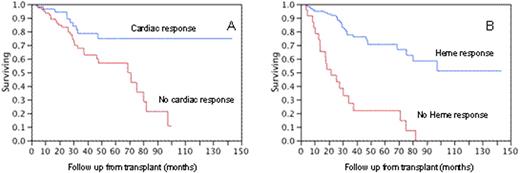
The median (range) age of pts at the time of SCT was 57.3 years (31-71); 122 (64%) were males. The median (range) duration from AL diagnosis to SCT was 3.6 mos (1-75). The estimated median follow up for the entire cohort was 44 mos (95% CI; 38-54) and 39 mos (95% CI; 32-51) from AL diagnosis and SCT, respectively. The estimated median overall survival (OS) for the cohort was 77 mos (95% CI; 38-86) and 69 mos (95% CI; 33-80) from AL diagnosis and SCT, respectively, and 107 (57%) pts were alive at the time of analysis. One, 2 or 3 organs were involved in 32 (17%), 106 (57%) and 50 (26%) pts, respectively. At the time of SCT, the median (range) septal thickness was 14 mm (9-25), and the median (range) EF was 63% (28-84). The cTnT/NT-ProBNP stage was availabel for 100 pts (6, 51 and 43 pts in stages 1, 2 and 3, respectively). Melphalan 200/m2 (85 pts) or Mel/TBI (10 pts) was used for conditioning in 51% pts, whereas the other half had reduced doses of melphalan (100-160 mg/m2). Thirty-one (16.5%) pts had died within 100 days of SCT. A hematologic response was obtained in 129 (69%) pts. A decrease in septal thickness was seen in 88 (47%) pts, with the median (range) decrease being 2mm (1-8). An increase in EF was seen in 85 (45%) pts and the median (range) increase was 6% (1-29). A conventional cardiac response (septal decrease > 2 mm or EF increase '20%) was seen in 62 (33%) pts. A decrease in NT-ProBNP was seen in 31 pts (90 with availabel values). The impact of hematologic or organ response on the OS from SCT was assessed only for those surviving beyond 100 days (landmark analysis). The median OS for those with a hematologic response (149 evaluable) was not reached (NR) compared with 22 mos for those with no response (P < 0.001) (fig B). The median OS for those with a conventional cardiac response was NR compared with 69 mos for those with no response (p=0.003) (fig A). The median OS for those with any decrease in NT-ProBNP was NR compared with 26 mos for those without any decrease (P<0.001). The best cutoff for NT-ProBNP decrease to predict pts being alive at 2 years was 55%, with all such pts alive at the time of analysis. A baseline troponin of <0.02 ng/ml or NT-ProBNP <5000 pg/ml best predicted the possibility of being alive at 1-year post SCT. Transient worsening of echocardiogram as well as cardiac biomarkers were seen in some pts who eventually improved. Eighty-one pts (43%) have died after SCT due to cardiac (37 pts) and non-cardiac (27 pts) causes; while the cause of death was not known in others.
SCT is an effective approach in pts with cardiac involvement due to AL, with hematologic and cardiac responses seen in over two-thirds and one-thirds of the pts, respectively. Improved survival is associated with hematologic and organ responses. Cardiac biomarker improvement may be used as a measure of organ improvement and correlates with outcome. This finding will need to be confirmed in a larger group of pts, as well as with other therapies for AL.
Lacy:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal