Abstract
Abstract 521
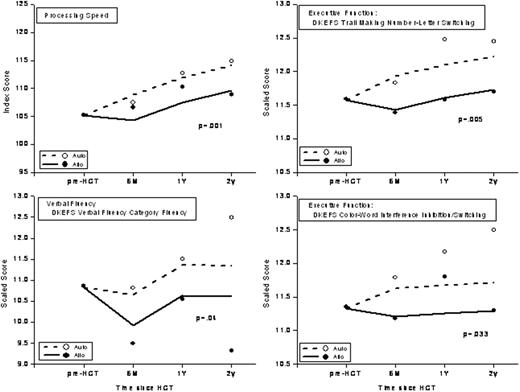
Patients undergoing HCT are at risk for neurocognitive impairment because of exposure to potential neurotoxic agents such as total body irradiation (TBI) and agents used for prophylaxis/ treatment of graft vs. host disease (GvHD). However, extant studies reporting neurocognitive outcome have been hindered by small sample size, retrospective or cross-sectional study design, limited prospective post-HCT follow-up, and restriction of study populations to either autologous or allogeneic HCT recipients, with inability to compare the two groups. Additionally, no prior studies have systematically assessed the impact of cognitive changes on the ability to return to work. This study addressed these gaps in knowledge by using a prospective longitudinal study design to examine neurocognitive changes from pre-HCT to 2 y after HCT in 284 patients undergoing HCT between 2005 and 2008. This study examined clinical and demographic predictors of neurocognitive function as well as the impact of neurocognitive function on return to part-time (PT) or full-time (FT) work post-HCT. Mean age at HCT was 50 years (range, 18-73); 40% were females; 69% were non-Hispanic whites and 21% were Hispanics. Primary diagnoses included NHL (33%), MM (26%), AML (16%), HL (10%), ALL (7%), and other (8%); 63% received autologous, 16% allogeneic related, and 20% unrelated donor HCT. A standardized 2-hour battery of neurocognitive tests was administered to the study participants at pre-HCT (n=284), 6 mo (n=202), 1 y (n=173), and 2 y (n=97) post-HCT to assess neurocognitive functioning in 8 domains: processing speed, executive function, immediate memory, general memory, working memory, psychomotor speed, verbal speed, and verbal fluency. The Wechsler Abbreviated Scale of Intelligence was used to measure cognitive reserve. Test scores were age-adjusted using normative data. Changes in neurocognitive functions over time and correlates of change were examined using the linear mixed effects model. Demographic factors examined included age at HCT, sex, race/ ethnicity, marital status, annual income at HCT, and education. Clinical factors included primary diagnosis, risk of relapse at HCT, stem cell source, presence of GvHD (for allogeneic HCT), conditioning (specific chemotherapeutic agents or TBI), and GvHD medications (allogeneic HCT only). Compared to pre-HCT, neurocognitive function generally remained unchanged or improved over the 2 years after HCT. At both pre- and post-HCT, higher cognitive reserve and education level were significantly associated with better neurocognitive function. Furthermore, women tended to have significantly better neurocognitive scores than men. However, after adjustment for significant covariates, allogeneic HCT recipients demonstrated significantly worse scores after HCT in processing speed, executive function, and verbal fluency when compared to autologous HCT recipients (p=0.001, p<0.05, p=0.04, respectively) (Figure). No differences were evident by GvHD status among allogeneic patients. Among patients who were employed prior to HCT, 66% were working either PT (27%) or FT (39%) at 1 y post-HCT. Patients with better scores in immediate memory (p=0.02), those who were either <35 y or >55 years of age at HCT (p=0.05), and those who had a primary diagnosis of lymphoma (p=0.03) were more likely to return to work either FT or PT. On the other hand, patients with chronic GvHD were less likely to return to work (p=0.02). Patients working FT at 1 y were more likely to have scored better for verbal speed (p=0.01); were more likely to have had pre-HCT income of $20,000 or more (p=0.002); and were less likely to have received allogeneic HCT (p=0.003). In summary, patients receiving allogeneic HCT are at risk for domain-specific neurocognitive deficits that persist for at least 2 years post-HCT and that are associated with inability to return to work. This study identifies vulnerable subgroups that could benefit from targeted surveillance and early intervention to facilitate smooth reintegration into society.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal