Abstract
Abstract 50
High dose chemotherapy followed by autologous stem cell transplantation (ASCT) has been shown to prolong progression free survival (PFS) as well as overall survival (OS) in patients (pts) with relapsed follicular lymphoma (FL). However, ASCT is usually not considered curative. Myeloablative allogeneic transplant has produced long term PFS in a subgroup of pts but is hampered by significant transplant related mortality (TRM). Reduced intensity transplant has less TRM but reports suggest a higher relapse rate. We therefore hypothesized that a tandem strategy consisting of ASCT followed by nonmyeloablative allogeneic transplant (NMT) would mimic a myeloablative allogeneic transplant without the associated early toxicity.
We initiated such a prospective protocol for pts with relapsed FL in 2003. Patients underwent ASCT with a chemotherapy based conditioning regimen; 3 months post ASCT, pts with a 6/6 related donor received an outpatient NMT with 5 days of fludarabine 30 mg/m2/d and cyclophosphamide 300 mg/m2/d followed by infusion of ≥4×106 donor CD34+ cells/kg. GVHD prophylaxis, selected to take advantage of the low incidence of acute and the putative protective effect of chronic GVHD (as we have previously published in BBMT 2009 Aug;15(8):919), consisted of tacrolimus 3 mg bid started on day (D)-8 to achieve levels of 10–15 nmol/L then tapered off by D+100 and mycophenolate mofetil 1 g bid from D+2 to D+50.
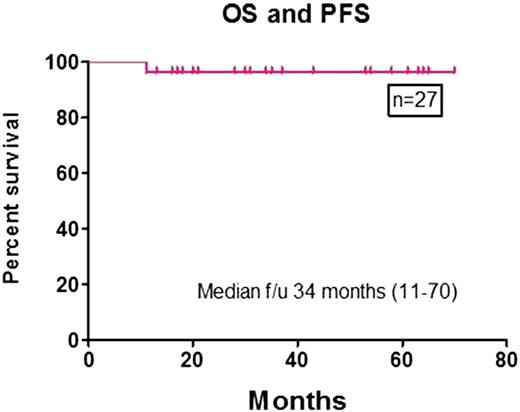
Between 4/2003 and 10/2008, 27 pts (M/F: 19/8) underwent tandem transplant, including 25 with FL and 2 with histology compatible with either FL or marginal zone lymphoma; 6/27 had histological progression towards an aggressive lymphoma. Median age was 49 years (range 34–65). The pts had previously been treated with a median of 3 lines of therapy (range 2–6). Median time from diagnosis to transplant was 34 months (range 14–131); 8 patients had never been exposed to rituximab. Disease status prior to ASCT was: 8 CR, 14 PR and 5 refractory. Conditioning chemotherapy for ASCT was: BEAC (n=14) and BEAM (n=13). 23 pts received peripheral blood stem cells and 4 received bone marrow for their ASCT. 2 pts received radiotherapy after ASCT to sites of previously bulky disease. Median time between ASCT and NMT was 133 days (range: 75–285). Pre NMT disease status was: 14 CR, 8 PR, 3 refractory, and 2 unknown. Median number of CD34+ cells/kg infused for NMT was 8.2 ×106 (range 3.2–29.2). Engraftment was prompt in all pts. 5 pts (18%) developed acute GVHD: 1 grade II and 4 grade III (2 classic acute and 3 delayed onset). Overall, 18 (67%) pts developed extensive chronic GVHD requiring treatment. Disease status at last follow up was: 22 CR and 5 unconfirmed CR. To date, there has been no disease progression and only 1 patient has died from GVHD at +11 months. With a median follow-up of 34 months (range 11–70) OS and PFS are both 96% at 3 and 5 years.
In conclusion: 1) ASCT followed by sibling NMT for relapsed FL appears to be safe and well tolerated. 2) Disease response and PFS are excellent even in refractory and transformed cases of FL. 3) This novel approach warrants further investigation in larger prospective studies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal