Abstract
Abstract 4988
Primary myelofibrosis is a chronic myeloproliferative disease characterized by connective tissue deposition in the bone marrow and extramedullary hematopoiesis commonly involving the liver and the spleen.
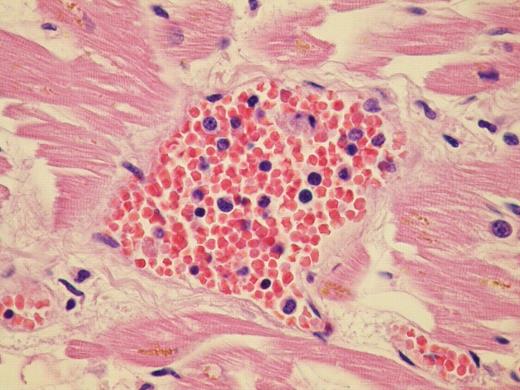
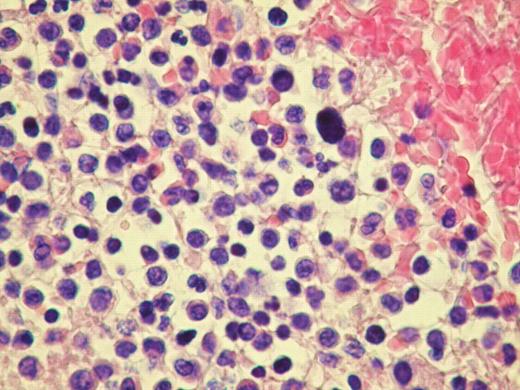
We report the case of a 60 year old patient with advanced Post Thrombocitemia Myelofibrosis extensively localized in almost all organs. He was referred to our Center in April 2008; clinical, radiological and haematological features suggested an evolution into Myelofibrosis. Molecular analysis for V617F JAK2 mutation was negative. Hemogram showed leukocytosis, mild anemia and normal platelet count. After few months of treatment with Danazol and Thioguanine, he was admitted for hemodynamic failure; echocardiography and chest X-ray were normal; abdomen CT scan confirmed important splenomegaly and didn't show any deep thrombosis. During hospitalization he developed massive intracerebral haemorrhage, cause of death. Post mortem histopatological examination documented osteomyelosclerosis and wide localization of extramedullary hematopoiesis. Morphological examination of the specimens showed an extensive dissemination of megakaryocytes, erythroid and myeloid precursors immunoreactive with factorVIII, hemoglobin, and myeloperoxidase respectively. We documented intravascular involvement of spleen, liver, lymph nodes, lungs, adrenal glands, myocardium, and central nervous system. Noteworthy fibrosis associated with haematopoietic cells were broadly distributed into retroperitoneal tissue.
Despite the massive myeloid metaplasia shown by the autopsy, general conditions of the patient until hospitalisation were good. Physical and radiological examination didn't reveal vascular and organ involvement. Although myeloid metaplasia is a possibility in advanced myelofibrosis, the assessment of cerebral and myocardial localization is difficult to find and standard radiological exams are not useful. In the subset of patients with Myelofibrosis and unexplained organ failure it could be interesting to look for an intravascular metaplasia throughout a multi-step approach: i) CD34+ peripheral cells count, since a very high count of these cells could suggest an extensive metaplasia; ii) high resolution pulmonary CT scan; iii) perfusional myocardial and/or pulmonary scintigraphy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal