Abstract
Abstract 4671
Infection after allo-Stem cell transplantation (SCT) is a major cause for post allo-SCT deaths. The pathogens involved are diverse and sometimes difficult to be distinguished. Treatment is primarily based on clinical history, blood analysis, chest X-ray, computerized tomography (CT) examination and pathogen culture of sputum or bronchoaleolar lavage fluid. Empirical treatment is often used before the results of pathogen culture are available. Here, we reported 2 cases of allo-SCT with similar clinical background but infections due to different pathogens.
| . | Case 1 . | Case 2 . |
|---|---|---|
| Age | 15 | 17 |
| Gender | female | male |
| Diagnosis | Acute lymphatic leukemia | Acute lymphatic leukemia |
| Genetic result | Normal karyotype | Normal karyotype |
| Immunological type | Common B cell | T Cell |
| Disease state before SCT | Complete remission | Complete remission |
| SCT type | Allo- peripheral blood SCT | Allo- peripheral blood SCT |
| SCT donor | Older sibling brother | younger sibling sister |
| SCT donor age | 18 | 15 |
| human leucocyte antigen (HLA) matching | Full match | Full match |
| Pretreated regimen before SCT | Classic regimen busulfanum + cyclophosphaminde (Bu/Cy) | Total-body irradiation (TBI) + Bu/Cy |
| Neutrophil >1.0×109/L days | +15 days | +21 days |
| Platelet >20×109/L days | +19 days | +23 days |
| Onset of the lung disease | 45 weeks after SCT | 62 weeks after SCT |
| Acute graft-versus-host disease (GVHD) | I∼II | II |
| Chronic GVHD | I | I |
| Anti-GVHD therapy | Cyclosporine A (CsA) withdrawal 3 months after SCT | CsA withdrawal 4 months after SCT |
| . | Case 1 . | Case 2 . |
|---|---|---|
| Age | 15 | 17 |
| Gender | female | male |
| Diagnosis | Acute lymphatic leukemia | Acute lymphatic leukemia |
| Genetic result | Normal karyotype | Normal karyotype |
| Immunological type | Common B cell | T Cell |
| Disease state before SCT | Complete remission | Complete remission |
| SCT type | Allo- peripheral blood SCT | Allo- peripheral blood SCT |
| SCT donor | Older sibling brother | younger sibling sister |
| SCT donor age | 18 | 15 |
| human leucocyte antigen (HLA) matching | Full match | Full match |
| Pretreated regimen before SCT | Classic regimen busulfanum + cyclophosphaminde (Bu/Cy) | Total-body irradiation (TBI) + Bu/Cy |
| Neutrophil >1.0×109/L days | +15 days | +21 days |
| Platelet >20×109/L days | +19 days | +23 days |
| Onset of the lung disease | 45 weeks after SCT | 62 weeks after SCT |
| Acute graft-versus-host disease (GVHD) | I∼II | II |
| Chronic GVHD | I | I |
| Anti-GVHD therapy | Cyclosporine A (CsA) withdrawal 3 months after SCT | CsA withdrawal 4 months after SCT |
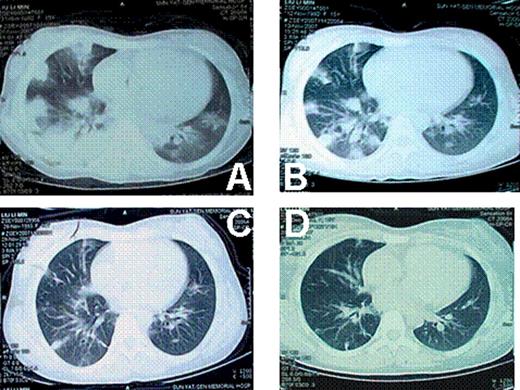
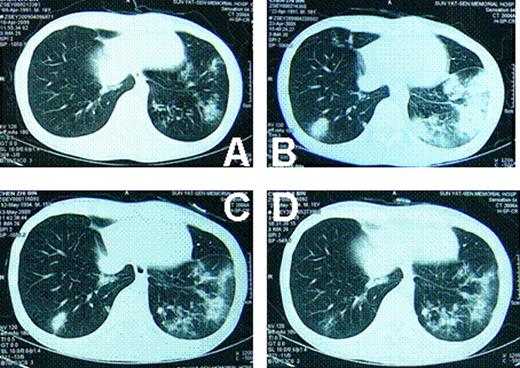
At the onset of the pulmonary diseases, anti-GVHD drugs (Including prednisone, CsA) were already withdrawn for both cases. There was no GVHD progression after withdrawal of the anti-GVHD drugs. Both cases had fever, ranging from 38 to 39 centigrade. Patients were short of breath. Oxygen inhalation was needed. Case 1 was in severe hypoxia. The oxygen saturation was down to 70%∼80% at the peak severity. Neither of the 2 cases was in need of mechanical ventilation. CT images showed that these 2 cases had similar lung injuries (Fig 1 and Fig 2). Tissue biopsy revealed that different pathogens were involved in these 2 cases, although they had identical disease history, similar duration after transplantation, same clinical symptoms and signs, even similar CT images. The histological findings of lung biopsies showed that the pathogen for case 1 was aspergillums, whereas that of case 2 was tubercle bacillus. Both cases responded well to the specific treatment, respectively. Patients are now in disease-free state.
Both tuberculosis and fungus infection could show diffused foci on CT image. The diffused lesions of tuberculosis tend to fuse, whereas little cavities were more frequently seen in fungus infections. After treatment, the lesions of fungus were much easier to be clear than tuberculosis. Diagnostic treatment might be used to distinguish these 2 diseases if biopsy cannot be performed or pathogen culture is negative.
lung CT of case 1. A: when the pulmonary infection began; B: 2 weeks later; C: 4 weeks later; D: 8 weeks later.
lung CT of case 1. A: when the pulmonary infection began; B: 2 weeks later; C: 4 weeks later; D: 8 weeks later.
lung CT of case 1. A: when the pulmonary infection began; B: 2 weeks later; C: 5 weeks later; D: 7 weeks later.
lung CT of case 1. A: when the pulmonary infection began; B: 2 weeks later; C: 5 weeks later; D: 7 weeks later.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal