Abstract
Abstract 3477
Poster Board III-414
Congenital afibrinogenemia (CA) is a rare bleeding disorder. While thrombosis is a recognized complication of dysfibrinogemia, the risk for thrombosis in CA has not been well studied. Life-threatening thrombosis with onset shortly after puberty has developed in 2 of 3 patients with CA followed through the coagulation program at The Children's Hospital, Colorado. Patient 1 suffered recurrent peripheral arterial thrombosis following cryoprecipitate administration during adolescence, massive myocardial infarction (MI) at age 19 years and death from spontaneous intracranial hemorrhage at age 20 years. Patient 2 has had superficial thrombophlebitis following intravenous (IV) infusion of fibrinogen concentrate, as well as bilateral pulmonary embolism with infarction 1 month following last infusion, without further recurrence over the course of 6 months of judicious use of anticoagulation and fibrinogen replacement. Patient 3 is 14 years old and receives fibrinogen replacement episodically for bleeding events, without thrombotic complications to date.
The object of this study was to investigate overall thrombin and plasmin generation potential and overall coagulative and fibrinolytic potential in CA, in order to generate hypotheses regarding pathophysiology of bleeding and thrombotic complications.
Plasma was collected from 2 CA patients at asymptomatic baseline states and following fibrinogen concentrate replacement. Plasma was isolated from whole blood within 1 hour, via double centrifugation at 2500 x g at 4°C x 15 minutes, and stored at -70°C until time of assay. Standard assays included fibrinogen activity by Clauss clotting assay and thrombin-antithrombin complexes (TAT) by ELISA (Siemens, Marburg, GE). Measurement of overall coagulative and fibrinolytic capacity in plasma was performed by Clot Formation and Lysis (CloFAL) global assay, as previously described (Goldenberg et al., Haemophilia, 2008). Simultaneous Thrombin and Plasmin generation assay (STP) was performed by fluorometric method with the same reagents as used in the CloFAL assay (dilute tissue factor, phospholipid, tissue plasminogen activator), as previously reported (Grunzke et al., J Thromb Haemost 2009 (abstract)).
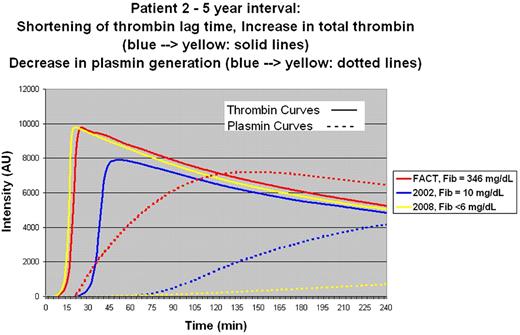
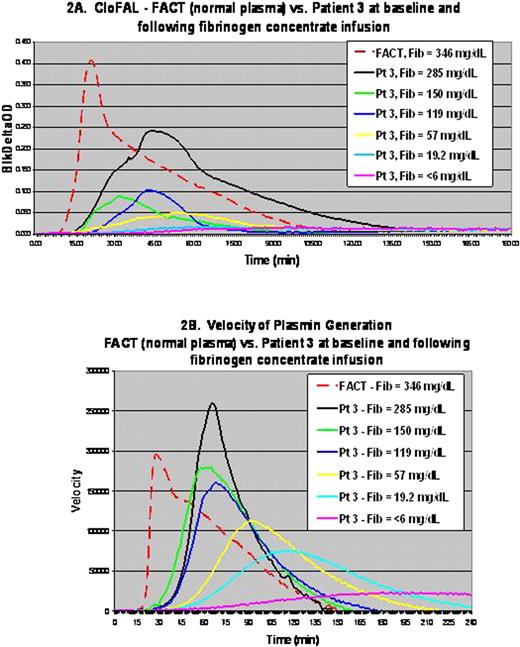
TAT was elevated to twice the upper limit of normal (9.4 mcg/L) in patient 1 six months following MI. In patient 2, TAT increased progressively from age 15 (2.9 mcg/L) to 20 years (13.7 mcg/L) while STP showed progressive shortening of time to peak thrombin generation by 60% over these 5 years (Figure 1). Baseline plasmin generation was nearly undetectable in both patients studied. As shown in Table I, TAT increased significantly at peak post infusion of fibrinogen concentrate in both patients evaluated during half-life and recovery studies. As shown in Figure 2, panels A and B, coagulative capacity by CloFAL assay and velocity of plasmin generation by STP showed dose dependence to fibrinogen following IV replacement with concentrate in patient 3.
| Patient 2: Time after fibrinogen concentrate (hrs) . | Fibrinogen (mg/dL) . | TAT (mcg/L) . | Patient 3: Time after fibrinogen concentrate (hrs) . | Fibrinogen (mg/dL) . | TAT (mcg/L) . |
|---|---|---|---|---|---|
| Pre-infusion | <5 | 4.5 | Pre-infusion | 19.2 | 1.5 |
| 0.5 | 84.5 | 27.0 | 1.5 | 285.5 | 2.1 |
| 1.3 | 78.8 | 3.0 | 48 | 119.1 | 1.6 |
| 24 | 47.0 | 2.2 | 96 | 57.0 | 1.7 |
| 48 | 35.7 | 1.8 | |||
| 72 | 26.5 | 2.2 | |||
| 144 | 13.0 | 2.2 |
| Patient 2: Time after fibrinogen concentrate (hrs) . | Fibrinogen (mg/dL) . | TAT (mcg/L) . | Patient 3: Time after fibrinogen concentrate (hrs) . | Fibrinogen (mg/dL) . | TAT (mcg/L) . |
|---|---|---|---|---|---|
| Pre-infusion | <5 | 4.5 | Pre-infusion | 19.2 | 1.5 |
| 0.5 | 84.5 | 27.0 | 1.5 | 285.5 | 2.1 |
| 1.3 | 78.8 | 3.0 | 48 | 119.1 | 1.6 |
| 24 | 47.0 | 2.2 | 96 | 57.0 | 1.7 |
| 48 | 35.7 | 1.8 | |||
| 72 | 26.5 | 2.2 | |||
| 144 | 13.0 | 2.2 |
These data suggest that baseline and post infusion thrombin generation may be increased in post pubertal patients with CA. Furthermore, given undetectable plasmin generation in the absence of fibrinogen, the hemostatic balance in CA is simultaneously hemorrhagic and prothrombotic. These preliminary findings call for further prospective evaluation in other identified patients with CA.
Grunzke:National Hemophilia Foundation/Baxter Clinical Fellowship Award: Research Funding. Manco-Johnson:CSL Behring: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal