Abstract
Abstract 3413
Poster Board III-301
Remission duration of less than 1 year following primary treatment for HL has been associated with poor prognosis following high dose therapy and autologous stem cell transplant (ASCT) in several published series; however these studies included patients treated with older HL regimens (Reece et al. 1994; Brice et al. 1996; Moskowitz et al. 2001; Josting et al. 2002). We investigated the outcome for patients transplanted following remission duration of less than 1 year after currently used primary chemotherapy regimens to identify risk groups who may benefit from post-transplant maintenance or consolidation therapy.
We combined data from 2 large transplant centers, Cleveland Clinic Taussig Cancer Institute (CCTCI) and Memorial Sloan Kettering Cancer Center (MSKCC), analyzing consecutive patients transplanted with chemosensitive disease for rel/ref HL following induction failure or remission durations of less than 1 year. Prognostic factors were determined using univariate and multivariate analysis. Review was carried out with approval of the respective Institutional Review Boards.
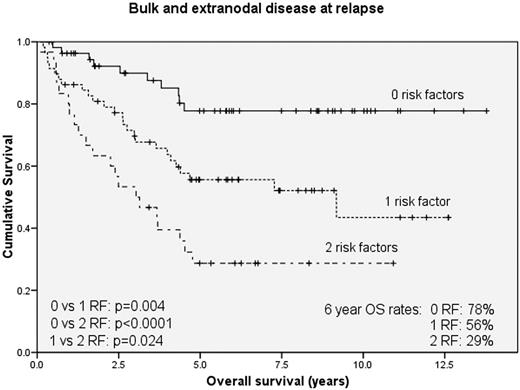
Two hundred and fourteen patients were included in this series; 112 patients from CCTCI transplanted between 1995 and 2008, and 102 patients from MSKCC transplanted between 1994 and 2005. The median follow up for survivors was 6 years. The group consisted of 49% females with a median age of 31. The majority (80%) received ABVD or Stanford V as induction therapy. Tandem transplants were performed in 39 pts (18%). Patients received a median of 2 previous chemotherapy regimens prior to transplant (range 1-4) and 64 (30%) received previous radiation therapy. One hundred and seven (50%) patients were primary induction failures, 127 (59%) failed induction or relapsed within 3 months of primary treatment, and 87 pts relapsed between 3 and 12 months. At relapse, 52 pts (24%) had a single nodal mass measuring greater than 5 cm, 91 pts (43%) had extranodal disease (ENS), and 51 pts (24%) had B symptoms. The EFS and OS at 6 yrs for all pts were 47% and 55% respectively. Factors significant for prognosis in univariate analysis were B symptoms, ENS, and bulk >5cm at relapse as well as remission duration less than 3 months and greater than 2 treatment regimens prior to transplant. In multivariate analysis, ENS and bulk remained significant for EFS and OS. We incorporated these two factors into a risk model separating patients into favorable (n=56), intermediate (n=58) and poor (n=30) survival groups. Figure 1 shows the OS for pts according risk groups.
Patients transplanted with remission duration less than 1 year for rel/ref HL have an OS rate at 6yrs of 55% which compares favorably to earlier transplant series. Furthermore, 39% of pts within our cohort had no ENS or bulk at relapse and had excellent outcomes with 6 yr EFS and OS of 63% and 78% respectively. Thus, patients with the sole risk factor of relapse within 1 year of induction therapy are expected to have favorable outcomes and should not be considered poor risk; however those pts with remission duration less than 1 year and concomitant ENS, bulk or both are excellent study candidates for transplant studies incorporating novel agents.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal