Abstract
Abstract 3386
Poster Board III-274
Previous studies have shown that rapid recovery of the absolute lymphocyte count (ALC) is associated with improved transplant outcomes after related and unrelated donor allogeneic stem cell transplantation (allo-SCT). Natural killer (NK) cells are the first lymphocytes to recover after allo-SCT and comprise the majority of peripheral blood lymphocytes after transplantation. Rapid recovery of NK cells at 1 month post allo-SCT has been associated with rapid neutrophil and platelet engraftment and decreased non-relapse mortality. Studies have shown that prolonged T-cell lymphopenia and compensatory expansion of B and NK cells occurs early after cord blood transplantation (CBT). However, no consistent link has been reported between lymphocyte/NK cell recovery and transplant outcome after CBT.
Records from 40 CBT patients at our institution (3/2006-6/2009) were reviewed to determine the impact of lymphocyte recovery on transplant outcome in an IRB-approved study. The ALC was calculated based on the total white cell count and automated differential. Common transplant outcome variables (graft failure, acute and chronic graft versus host disease [GVHD], relapse, non-relapse mortality [NRM] and survival) were studied in relation with ALC at 1, 2, 3 months post-CBT. ALC was analyzed as a continuous variable and also as a dichotomous variable with two distinct groups based on transplant associated outcomes.
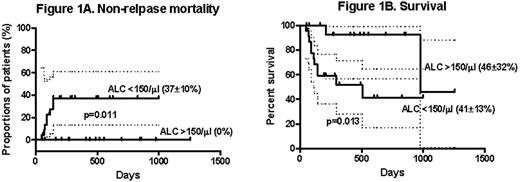
The majority of patients (n=33, 83%) received CBT for hematological malignancies. The median age was 22 years (range: 0.6-64), and 24 (60%) were male. Disease status at transplantation included 29 (73%) high risk and 8 (20%) standard risk hematological malignancies. Conditioning consisted of myeloablative regimens in 28 (70%) (TBI=21, non-TBI=7). Fifty percent of patients received thymoglobulin with their conditioning regimen. All patients received calcineurin inhibitors and mycophenolate for GVHD prophylaxis. Nineteen patients (48%) received two cord blood units. The median nucleated cell dose was 4.1 × 10 7 cells/kg (range, 2.2-27.3). Five (13%) patients experienced graft failure. Acute GVHD (grade II-IV) occurred in 30 (75%) patients; chronic GVHD occurred in 15 of 31 patients (48%) surviving beyond 100 days. Six (15%) experienced relapse and 9 (23%) died from non-relapse causes. At the time of analysis, 26 patients (65%) were alive with a median follow-up for surviving patients of 422 days (range 51-1256). Patients with ALC<100/μl at 1 month post-CBT showed increased graft failure (4 of 10 vs. 1 of 29; p=0.011). Patients with ALC>150/μl at 1 month post-CBT had decreased NRM (0 vs. 37%±10%, p=0.011) and improved survival (46%± 32% vs. 41%±13%, p=0.013) (Figure 1). There was no impact of ALC at 1, 2, or 3 months post-CBT on relapse or acute or chronic GVHD. There was no relationship between age, type of conditioning regimen, disease risk, number of cord units (one vs. two) or nucleated cell dose on ALC recovery.
Our results indicate that ALC 1 month post-CBT is a surrogate marker for engraftment, and that low ALC (<150/μl) identifies an “at-risk” population of patients after CBT. These results point to the importance of developing patient-specific strategies to improve outcomes in those who fail to achieve satisfactory lymphocyte counts in the first month post-CBT. A limitation of this study is the small sample size, and validation in larger prospective multicenter CBT studies is warranted.
Jagasia:Genzyme: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal