Abstract
Abstract 3372
Poster Board III-260
Although Hodgkin lymphoma is usually characterized by a high chemosensitivity and a good prognosis, a minority of patients with primary refractory disease or early relapse after intensive chemotherapy presents poor outcome (Brice. British Journal of Haematology 2008 ; 141 : 3-13. Moskowitz. British Journal of Haematology 2009 ; 146 : 158-163). AlloSCT is one of the treatment-options that can be proposed for these progressive patients but the optimal management remains controversial because comparative studies are lacking. However, several groups report encouraging survival results with acceptable non relapse mortality after alloSCT with reduced intensity conditioning.
We retrospectively studied 31 patients who received an alloSCT in Saint-Louis Hospital, Paris. The aim of the study was to compare their outcome with those of patients with similar characteristics who did not receive alloSCT. In order to have an homogenous group of patients, we only compared patients who relapsed after an autologous SCT (autoSCT) and were alive at least 12 months after autoSCT. To correct the recruitment bias, the propensity score (PS) methodology was used to determine the probability of receiving alloSCT in the group of patients who relapsed after autoSCT, according to a set of baseline characteristics (Rosenbaum. Biometrika 1983;70:41-55). Parameters used for this PS score were age, primary chemorefractory disease and stage III-IV at first relapse. This PS was estimated using logistic regression and used to match 1:1 patients with similar propensity to receive alloSCT, based on the nearest neighbor matching using calipers of width 0.2.
AlloSCT recipients characteristics: Thirty-one patients (19 males and 12 females) received an alloSCT between 2000 and 2007. Median age at alloSCT was 26 years. Median number of previous lines of chemotherapy was 3.6 (range from 2 to 7) and 28 (90%) patients were previously autografted. 13 (42%) were considered refractory to primary treatment and 11 (35%) to secondary treatment. Status at alloSCT were: 20 (65%) patients in CR, 9 (29%) in PR and 2 (6%) in progressive disease. Pre-transplant co-morbidity score was 0 in 26 (84%), 1 in 3 (10%) and 2 in 2 (6%) patients. 26 (84%) patients received a reduced intensity conditioning regimen and TBI was performed in 23 (74%) recipients. Most of the patients (n=24, 77%) received peripheral stem cells and donors were HLA-identical siblings in 15 (48%) cases. Median follow-up after autoSCT and alloSCT was 62 and 51 months respectively. All patients engrafted. Grade II-IV acute GVHD occurred in 10 (32%) patients. Chronic GVHD occurred in 13 (42%). Three months after alloSCT, 19 patients were in remission, 5 presented stable disease and 7 were progressive. Eleven patients relapsed despite alloSCT and 11 patients died. The estimated 3-year overall and event free survival were respectively 69% (95% CI [48;82]) and 41% (95% CI [23;58]) and 3-year non relapse mortality was 21% (95% CI [13;29]). Causes of death after alloSCT were: progression in 6 (55%) and toxicity in 5 (45%) patients.
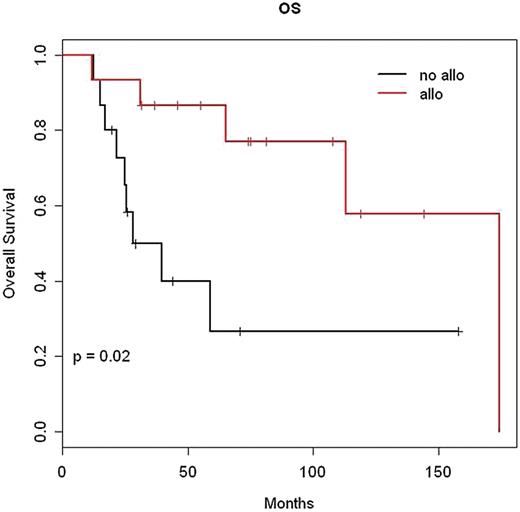
From the 31 alloSCT recipients, 15 matched pairs were successfully constituted according to the PS. As expected, the distribution of age (p=0.97), stage III or IV at relapse (p=0.67) and primary chemorefractory disease (p=1) were not different between patients treated by alloSCT and untreated subjects. Based on these matched pairs, the estimated hazard ratio of death was 0.24 (95% CI [0.07;0.80]) for allografted patients compared with non allografted.
In conclusion, alloSCT in poor-prognosis Hodgkin lymphoma gives promising survival outcomes although performed in advanced disease and provides survival benefit with acceptable non relapse mortality in comparison with non allograft treatment as suggested by PS method.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal