Abstract
Abstract 3337
Poster Board III-225
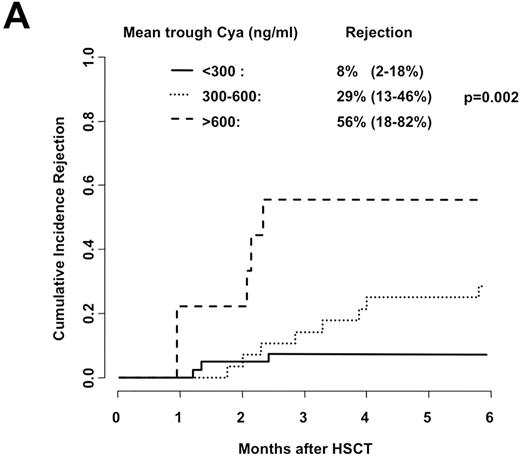
In the past decade there has been a significant increase in the use of reduced intensity conditioning (RIC) regimens for allogeneic hematopoietic stem cell transplantation (HSCT). RIC HSCT is associated with reduced transplant related mortality, but also with an increased risk of relapse and graft rejection. Little is known about factors associated with graft rejection. Based on early animal models, intensified cyclosporine (CyA) administration is considered an essential component of RIC HSCT with minimal conditioning. We were interested in analyzing the role of CyA in graft rejection following RIC HSCT. Between October 1999 and December 2008, 85 patients received an allogeneic RIC HSCT with fludarabine 3 × 30 mg/m2 and 2 Gy TBI as conditioning at our institution. 6 patients were excluded from the analysis due to graft loss associated with relapse or progressive disease, 2 were excluded for missing data. Diseases were acute leukemia (N=19), MDS (N=11), CML/MPN (N=10), lymphoma (N=24), multiple myeloma (N=12), and pure white cell aplasia (N=1). Donors were HLA-identical siblings (N=54) or unrelated donors (N=23). Graft source was peripheral blood (N=74) or bone marrow (N=3). Graft-versus-host disease (GvHD) prophylaxis consisted of CyA and mycophenolate mofetil (MMF). CyA was started at a dose of 6.25mg/kg p.o. twice daily and adjusted according to trough levels (measured weekly) and toxicity. MMF was administered at a dose of 15mg/kg twice daily; trough levels were not analyzed systematically. For the analysis of impact on graft rejection, CyA levels between day 1 and 28 where summarized as mean trough levels. Graft rejection was defined as <5% donor cells at any time on day 28 or later or application of donor lymphocyte infusion for declining donor chimerism. Of the 77 evaluable patients, 16 (21%) experienced graft rejection at a median of 69 days after transplantation. There was no significant difference in disease stage (early vs. advanced), median age at transplant (56 and 57 years, respectively), EBMT risk score, graft cell count (nucleated and CD34+ cells) and history of previous transplants between patients with or without rejection. In contrast, there was a significant difference in underlying disease, with a higher proportion of CML/MPN and a lower proportion of multiple myeloma in rejecting patients. Mean CyA trough levels were clearly associated with graft rejection with a cumulative incidence of rejection of 8%, 29% and 56% with trough levels of <300 ng/ml (N=40), 300-600 ng/ml (N=28) and >600 ng/ml (N=9) (p=0.002) (Figure A) and a median donor chimerism at day 28 of 99%, 84%, and 72% respectively (p=0.004). In a multivariate analysis, two factors remained significantly associated with graft rejection: unrelated donor (HR vs. sibling donor 4.52, p = 0.03), and mean trough level of CyA for days 1-28 (HR 1.006 per ng/ml increase, p=0.001). Patients with CML/MPN had an increased risk of rejection (HR 1.36 versus other patients combined, p=0.65) which did not reach statistical significance. The overall survival of the entire patient group was 55% at five years; patients with stable engraftment had a five-year survival rate of 61%, those rejecting their graft 36% (p=0.04). These data indicate that elevated CyA levels during the first month posttransplant might be associated with an increased risk of graft rejection. The potentially detrimental effects of high CyA levels have been described previously in the myeloablative setting, where a correlation between CyA levels and risk of relapse has been shown. Further studies will be needed to better define the exact role of CyA following RIC regimens.
Gratwohl:Amgen: Research Funding; Bristol Myers Squibb: Research Funding; Pfizer: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; Roche: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal