Abstract
Abstract 3325
Poster Board III-213
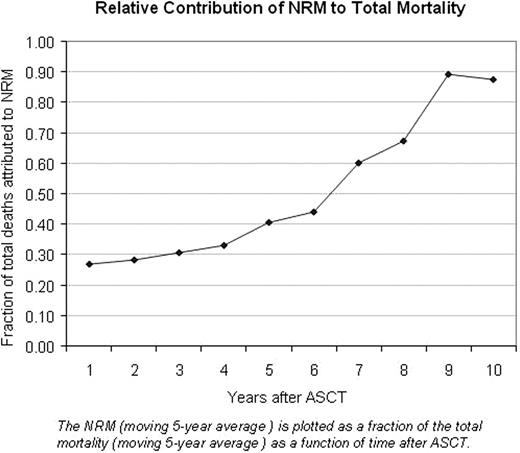
For patients with diffuse large B-cell lymphoma (DLBCL) who failed to achieve complete remission (CR) or who relapsed after obtaining CR with initial treatment, salvage therapy has historically resulted in poor long-term survival. The PARMA trial identified high dose chemotherapy followed by autologous stem cell transplantation (ASCT) as a superior treatment modality compared to standard chemotherapy. As originally reported in 1995, the 5-year event-free-survival (EFS) was 46% in patients undergoing ASCT, compared to 12% in patients receiving chemotherapy alone. Subsequent to the widespread adoption of ASCT, it has been noted that patients who have undergone autologous transplantation for relapsed or refractory DLBCL may be at increased risk of mortality well beyond 5 year point which has generally been an accepted surrogate for long-term survival. To assess long-term outcomes of these patients, we retrospectively analyzed data from 309 consecutive patients who received ASCT for DLBCL at the Cleveland Clinic from January 1994 through December 2006. Inclusion criteria were age ≥ 18 years, diagnosis of DLCBL, and history of a single autologous stem cell transplant. The median age of these patients was 51 years (range 19-72) and 61.2% were male. The median time from diagnosis of DLBCL to transplant was 14.7 months (range 2.1-372.3). 99.0% of patients received peripheral blood stem cells and 98.4% received a preparative regimen with busulfan/cyclophosphamide/VP16. As shown in the accompanying figure, non-relapse mortality (NRM) becomes the major cause of death approximately 6 years after ASCT. The most common causes of NRM during the study period were pulmonary toxicity (31%), infection (17%), cardiac toxicity (15%) and secondary malignancy (15%). In multivariate analysis, the strongest predictor of relapse mortality was disease status at transplant: patients who were in second complete or partial remission had a higher risk of relapse mortality than those in first complete or partial remission (hazard ratio [HR] 3.70, P<0.001), as did those who were relapsed or refractory (HR 4.85, P<0.001) Significant risk factors for NRM were older age (HR 1.43, P=0.017 per 10 year increase), prior chemotherapy (HR 1.31, P=0.030 per 1 regimen increase), and poor performance status at the time of transplant (HR 4.66, P=0.010 for KPS 50-80 relative to KPS 100).
In conclusion, we describe the longest reported follow-up of a large cohort of DLBCL patients uniformly-treated with ASCT. We have found that although relapse is initially the more likely cause of death, after six years, NRM exceeds relapse mortality. As more patients with DLBCL survive ASCT, these findings emphasize the need for active surveillance for causes of morbidity and mortality other than relapsed lymphoma.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal