Abstract
Abstract 3312
Poster Board III-200
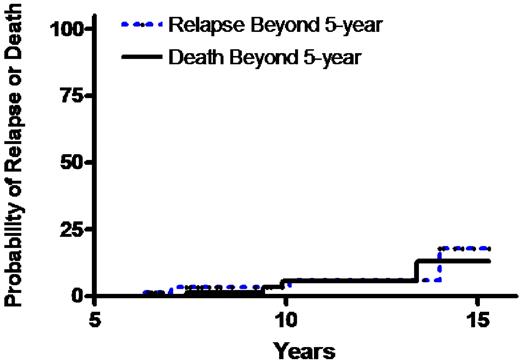
Allogeneic hematopoietic stem cell transplantation (SCT) is a curative treatment for some hematological malignancies. The ultimate measure of success of allogeneic SCT for hematological malignancies is its ability to eradicate malignant disease and restore a good quality of life (QOL) in long-term survivors. As numbers of survivors continue to increase, studies systematically examining outcomes in this group of survivors are needed. We studied the clinical and QOL outcomes in a large cohort of patients with hematological malignancies surviving 5 or more years after allogeneic SCT from a single institution. In 2005 we initiated a long term follow up protocol to further study complications in survivors after allogeneic SCT. Patients were enrolled at the third annual visit after transplantation. Annual follow-up visit includes comprehensive clinical evaluation and detailed assessment of QOL, symptom distress, physical and mental health. Measures for QOL included the Functional Assessment of Cancer Therapy-General (FACT-G), the Physical and Mental Component Summary scales (PCS, MCS) of the Medical Outcomes Short-Form 36 (SF-36), and the Rotterdam Symptom Checklist (RSCL). Two hundred sixty two patients with hematological disorder received a SCT from an HLA identical sibling since 1993. One hundred and twenty one patients (46 %) survived 3 or more years and were eligible for participation in the long-term evaluation protocol. Ninety two (35%) survived beyond 5 years from SCT (median follow-up 9.4 years, range 5.1-15.3) and were included in this analysis. Median age at transplantation was 35 years (range 10 - 56). Twenty-two (24%) received a bone marrow transplant, and 70 (76%) received a peripheral blood SCT. We examined chronic graft-versus-host-disease (cGVHD), disease relapse, survival and QOL. Seventeen (18%) of 92 survivors had active cGVHD (limited 9, extensive 8) and were receiving prolonged immunosuppressive treatment 5 years following allogeneic SCT. Four relapsed with leukemia, at a median of 8.5 years (range 6.2 -14.0) post SCT. Four (4.3%) died between 7.4 -13.4 years post SCT (1 relapse, 1 lung cancer, 1 pneumonia, 1 brain hemorrhage). Sixty (65%) completed QOL measures. Most survivors beyond 5 years had an excellent performance status with no difference in the PCS (p =0.89) and MCS (p =0.15) scores and higher FACT-G scores compared with population norms (p =0.02). Although the overall distress for physical and psychological symptoms was low, higher levels of symptom distress were associated with impairments in QOL. In eleven survivors with cGVHD, there was no statistical difference across QOL outcomes although the difference was meaningfully lower (≥5 points). In conclusion, five or more years after SCT for hematological malignancy most individuals survive disease free with an excellent performance status, preserved physical and psychological health, and excellent QOL. However patients with leukemia appear to have a persistent but low chance of disease recurrence. Although cGVHD persists in about 20% of patients it did not appear to affect the excellent QOL that most of our patients experience. The association between cGVHD severity and specific cGVHD manifestations and QOL outcomes requires further study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal